COVID focus
A quick look at pandemic-related news
Since the coronavirus pandemic arrived in the San Francisco Bay area and stay-home orders were issued, Stanford Medicine has been a crucial player in the battle against COVID-19, the disease caused by the virus.
What follows are three stories that reflect the voices of the people on the front lines with patients, the research behind diagnosing and treating the disease, and the care that is helping save lives.
A pandemic residency
Throughout the pandemic, medical residents at the front lines have been crucial players in patient care.

Gabriela Spencer, MD, was a night resident when Stanford Hospital received one of its first COVID-19-positive result for a patient.
The challenges of keeping health care workers, staff and patients safe were instantly clear, spurring Spencer to help design and distribute training materials for safety protocols and proper personal protective equipment use for other residents.
As the pandemic continued and hospital visitors were restricted, residents became crucial intermediaries between patients and families.
“It sometimes took a few hours just to make calls to the families, keeping them up to date in a very distressing situation,” said Spencer.
“I’m from Puerto Rico, and a lot of my patients were Spanish speaking. It’s really important for me to be able to have these sometimes charged and difficult conversations with their family members in their native language.” — Read the full story here.
A son’s fight to save his father
A desperate search to secure a transplant for his dad leads 24-year-old to Stanford Medicine.
Month after month, as his father, John, suffered the devastation that COVID-19 can inflict, 24-year-old Patrick kept watch.

By May, John was on life support and needed a lung transplant to survive, but his doctors in Washington said he was too weak for surgery, said Patrick, whose family didn’t want their last name used.
Patrick didn’t give up, though, and called transplant centers around the country. Many said no, but Stanford Health Care left a door open. If John could regain some strength, the hospital would fly him to Palo Alto to see if its doctors could help. So Patrick pushed for more physical therapy and kept encouraging his dad.
In August, John was able to board an air ambulance for Stanford. “That was a glorious day,” Patrick said. John’s kidneys had failed, but lungs and a kidney soon became available.
Overnight on Sept. 10-11, John underwent successful lung and kidney transplants, making him among the first COVID-19 patients to undergo a multiple-organ transplant. — Read the full story here.
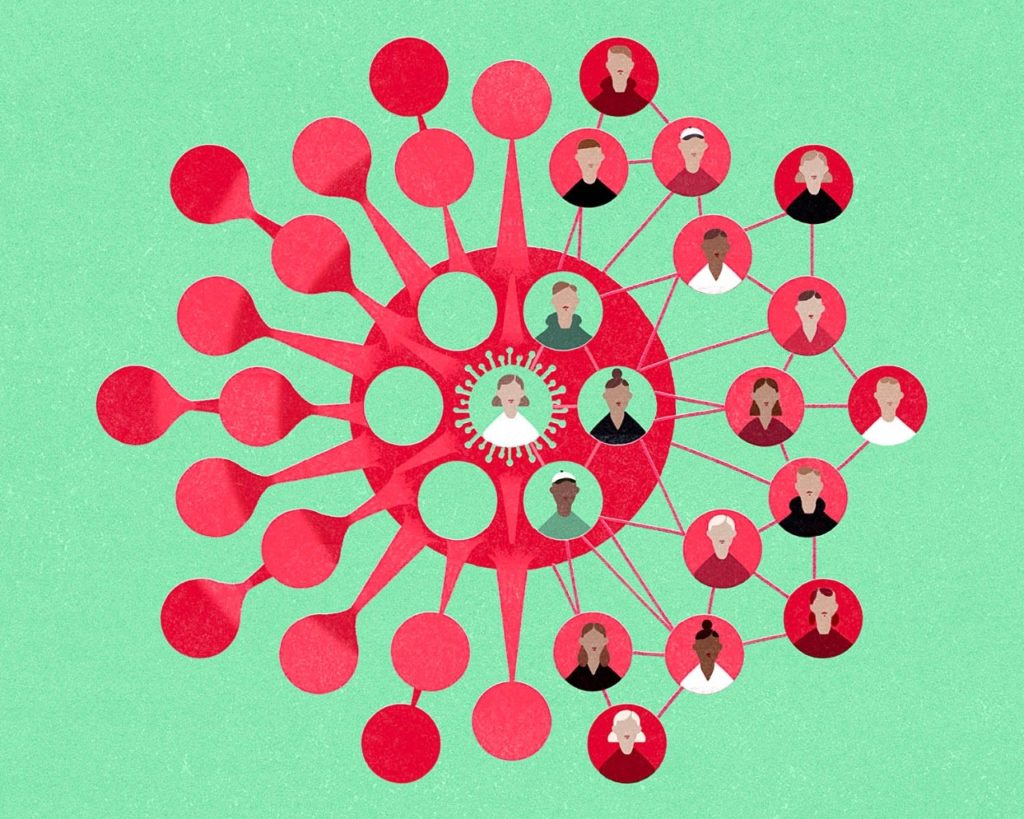
Tracking COVID mutations
Stanford Medicine researchers with COVID-19 diagnostics expertise are helping track and identify varients the coronavirus, which they say are key steps to stopping the spread of the virus.
Using the expertise that made them a leader in developing COVID-19 diagnostic tests, Stanford Medicine researchers are now tracking the spread of new mutations, or variants.
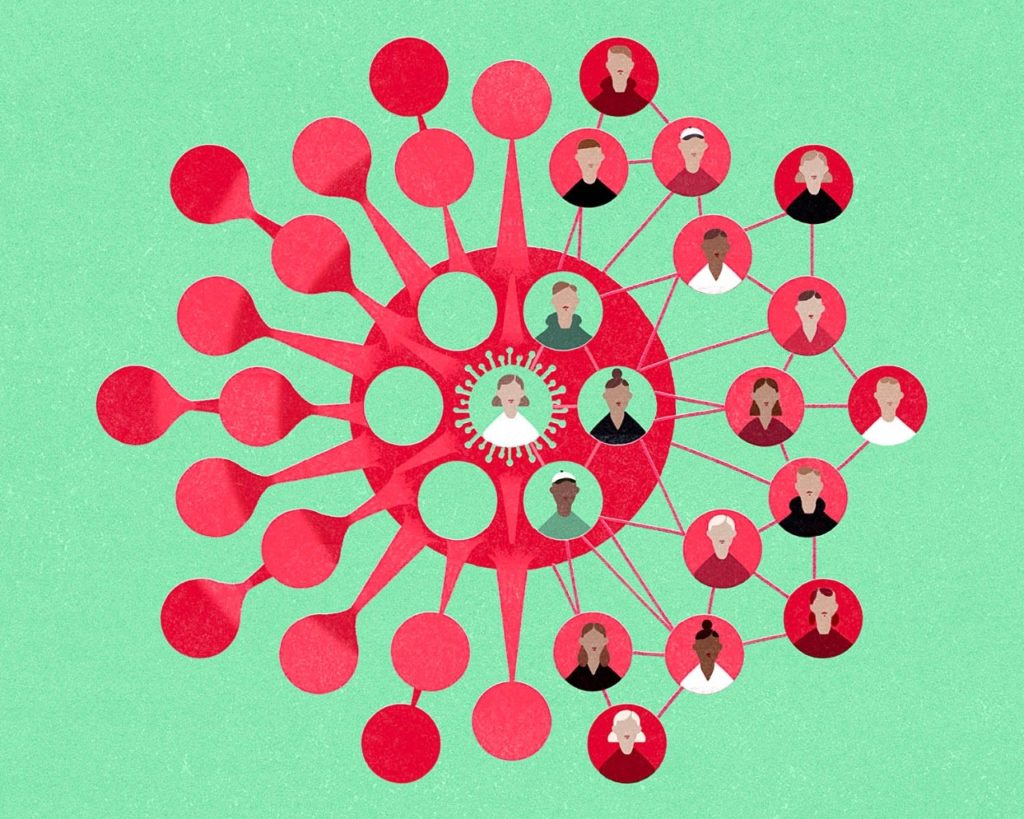
Testing at Stanford’s Clinical Virology Laboratory, led by the lab’s medical director, Benjamin Pinsky, MD, PhD, enables large-scale screening of diagnostic samples to track strains of the virus throughout California.
“In most cases it is too early to say whether or how these variants will influence the course of the pandemic, but it is important to monitor their evolution and spread,” said Pinsky, associate professor of pathology and of infectious diseases at Stanford’s School of Medicine.
Stanford uses a technology called reverse transcription polymerase chain reaction, or RT-PCR, to identify viral genetic material in samples collected from nasal passages. It helps researchers discern whether someone is infected and pinpoint whether they’re carrying the original coronavirus strain or a new variant.
Tracking variants and quickly identifying mutations is critical to understanding whether they will spread more easily, cause more-severe disease or render vaccines less effective. — Read the full story here.
