Vaccine hunter
The life and times of Jonas Salk
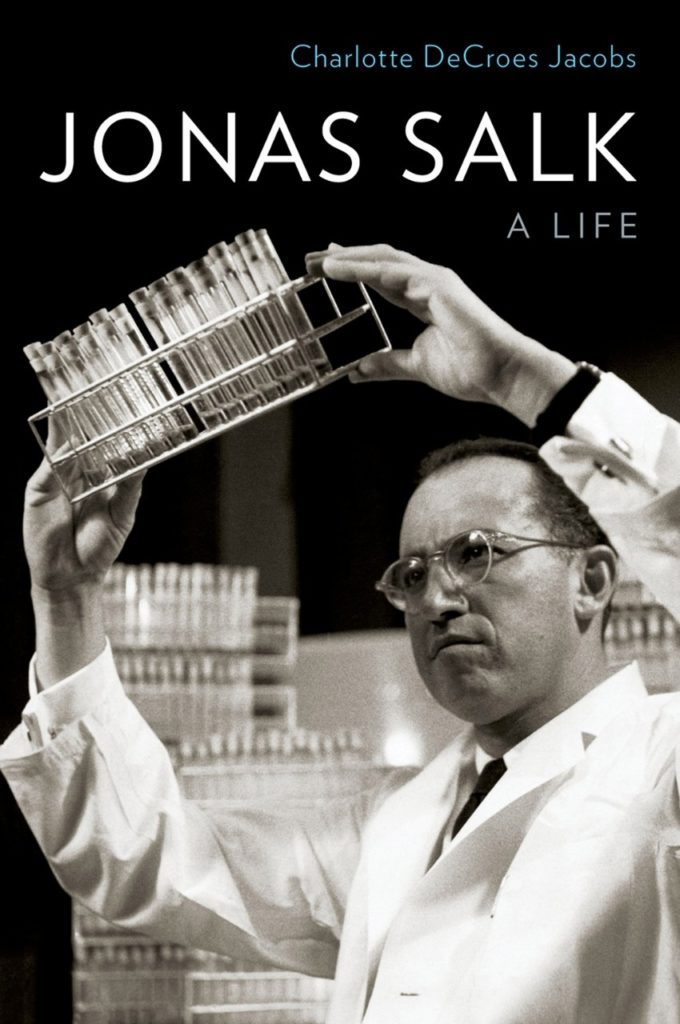
An excerpt from Jonas Salk: A Life by Charlotte Jacobs
Reprinted with permission from Oxford University Press Inc.
In the summer of 1916, New York’s playgrounds stood empty. No children splashed in public swimming pools; none sold lemonade on the sidewalks.
No cats roamed the alleys, peering into garbage cans. Troops of sanitary workers in white uniforms hosed down the city streets. Fathers hurried home from work, fear imprinted on their faces, averting their glances from the tiny wooden caskets lined up outside the tenements. Policemen patrolled the streets. New York was a city under siege.
Poliomyelitis had crept into Brooklyn while the public was busy watching the war unfold in Europe. It smoldered for a while between Henry Street and Seventh Avenue. Health officials barely paid attention, assuming it would soon die out. But it didn’t. When the press began to attach names and faces to the disease, the community became alarmed. Helen Downing, paralyzed just before graduation from Public School No. 134, received her diploma in bed. After 5-year-old Frederick Chaplin made his kindergarten’s honor roll, his brother took him to Coney Island. Five days later, he was dead.
Before long, the names and faces gave way to numbers, and they kept escalating. On June 28, Health Commissioner Haven Emerson announced that Brooklyn might be experiencing an epidemic. Although a scientist had identified the poliovirus eight years earlier, no one knew how it spread. Assuming it behaved like other contagious diseases, the commissioner ordered every family bearing a case quarantined. A placard was placed in the window; bed linens and clothing were disinfected; windows were screened to prevent flies from disseminating the disease. Street cleaners worked overtime to collect garbage and cleanse tenement halls and stairwells. Stray cats, suspected of harboring the virus, were rounded up and exterminated — 72,000 by summer’s end. The commissioner closed playgrounds and banned children from theaters. He instructed parents to keep food covered and to wash their youngsters’ noses and throats with saltwater daily. But filth and flies and cats had nothing to do with the spread of poliomyelitis, and even with these precautions, more children contracted the disease.

The illness started innocently enough — a sore throat, a runny nose. At the end of the day, the child spiked a fever, became restless. Then the pains began — electric shocks that darted through the back, legs, neck and shoulders. Muscles twitched, and spasms twisted him into a peculiar posture, the shoulders pulled forward, hips rotated, toes pointing downward. All night, the child thrashed about in his bed, drenched in sweat; his face became pallid. When the fever broke, he appeared to be recovering — a deceitful interlude as poliovirus left the bloodstream and invaded the nervous system.
Within a day or two, paralysis struck as abruptly as the fever had, and no one could predict the nature of its onslaught — a weak leg which improved in a few days or an arm dangling useless forever. Poliomyelitis impaired motor control of either one muscle or a group of muscles, yet it left sensation intact. The puzzled child could feel his feet but not move them. Three-quarters of those afflicted survived, many condemned to life in a wheelchair, on crutches or in bed. They joined a generation of cripples.
If the poliovirus attacked the nervous system higher up, in the base of the brain, death soon followed. Paralyzed throat muscles impeded swallowing. A sip of water streamed out the youngster’s nose or drained into his windpipe, causing him to sputter and cough. Unable to swallow saliva, he foamed at the mouth. Breathing gave way to gurgling. As his mother wiped the blood-tinged froth from his lips, he gasped for air, drowning in his own secretions. The struggle over, his eyes rolled back, followed by a few muscle jerks, and the mother held her lifeless child.
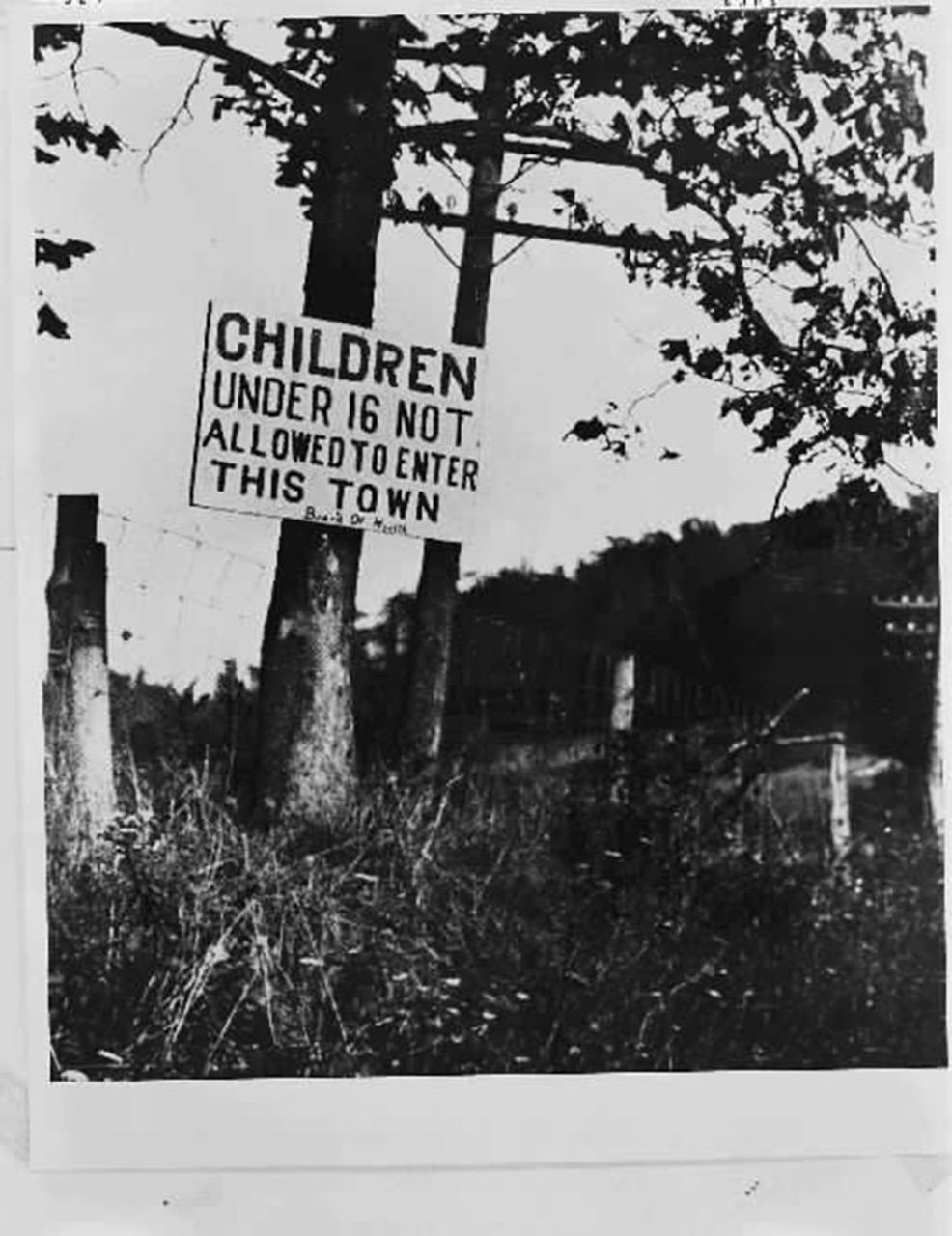
Poliomyelitis seemed to have a predilection for striking infants and toddlers. During the second week of July, 412 new cases were reported in New York; the next week, 712. Terrorized parents watched the figures more closely than the stock market. The disease erupted in Staten Island, Manhattan, the Bronx; it didn’t distinguish between immigrants and the upper class. Those who could fled. Mothers swarmed into Grand Central Station and the ferry docks, dragging their children into the crowds they should have avoided. The exodus of almost 1,200 children a day halted when towns began to bar them. In Hoboken, New Jersey, guards patrolled city entrances. Policemen blocked 150 families trying to enter Hastings-on-Hudson. Distraught, they returned to New York, where the death toll continued to rise.
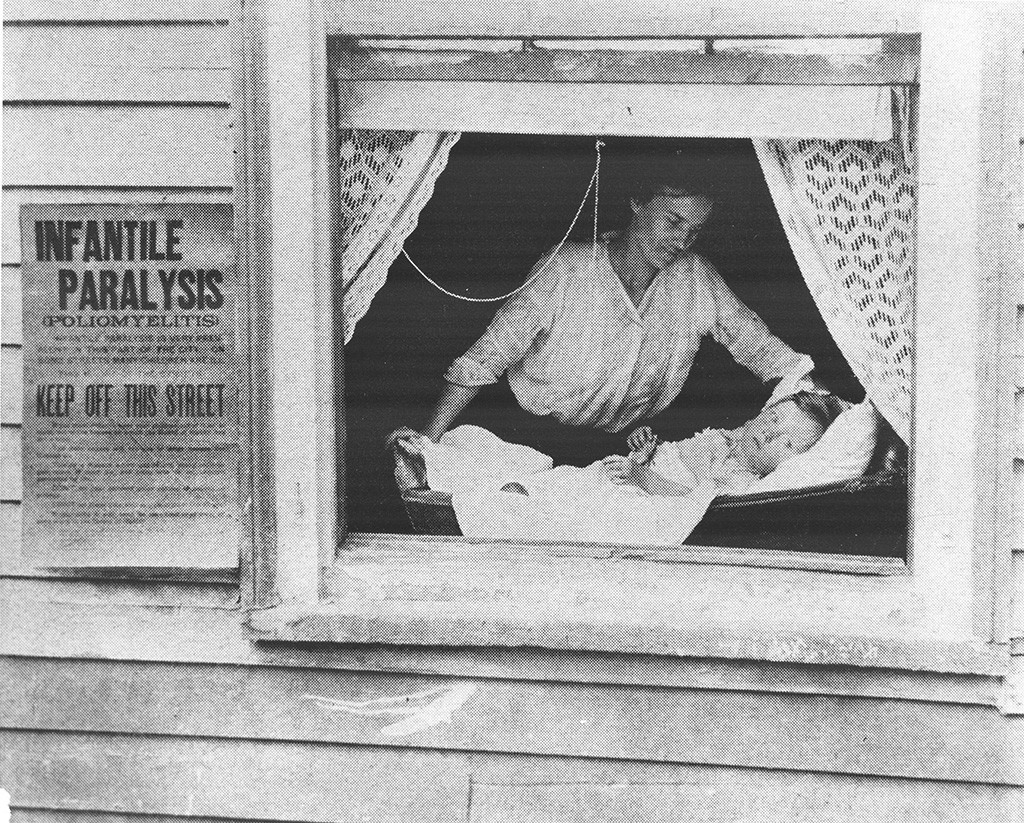
Families unable to afford medical assistance at home were ordered to deliver their infected children to Brooklyn’s Kingston Avenue Hospital for Contagious Diseases, where they were held in isolation for eight weeks. Prohibited from visiting, parents heard stories of hallways lined with metal cribs, children crying out in pain or pleading for water with no one to hold them. A knock at the door and a telegram notified parents to come retrieve their child’s body. When parents looked up at the dark, looming fortress of Kingston Avenue Hospital, many turned away, hiding their youngsters at home. But once a public health nurse discovered a poliomyelitis case in a neighborhood, the Sanitary Squad conducted a house-to-house search for others. Watching a policeman snatch a child from her mother’s arms reminded some of the pogroms that they had fled.
By August, every isolation bed in New York was occupied; many held three children. A baby died approximately every two and a half hours. Fear, bordering on hysteria, permeated the city. Then, when the weather turned cool, poliomyelitis disappeared just as unexpectedly as it had come. In America’s first major poliomyelitis epidemic, the poliovirus had infected approximately 8,900 in New York, leaving 2,400 dead and many of the remainder paralyzed. Nationwide it had afflicted 27,000, mostly children under 5 years of age. For the next 40 years, the carefree spirit of summertime was marred by the specter of this disease, now known simply as polio. Two years later, another disease ravaged New York — influenza.
In 1917, with the country preparing to join the war in Europe, reports of a few cases sounded no alarm. Outbreaks occurred every winter. Characterized by fever, muscle aches and intense exhaustion, the disease usually ebbed in a week, posing a threat mainly to the elderly and infirm. But in the fall of 1918, influenza metamorphosed into a vicious monster. With no warning, a previously healthy person complained of an excruciating headache, like a demon pounding his temples with a hammer, stabbing his eyes. A temperature spike up to 105 degrees ushered in agonizing muscle pains, profuse sweating and shaking chills. When the fever broke and relief seemed at hand, the coughing began. Mild at first, the cough deepened; the sputum turned bloody. A viscous fluid filled the lungs, and the patient gasped for breath, suffocating. No longer did it prey on the elderly; they seemed to be immune. Instead, this virulent form of influenza picked young, healthy adults as its victims.
No one was prepared for its fury. Initially the military was the hardest hit as overcrowded camps and close quarters aboard ships favored its rapid transmission. In September, more than 12,000 soldiers at Camp Devens, outside Boston, contracted influenza. Before long, it spread to civilian populations. As the point of embarkation for troops, New York felt the brunt of the disease early on. The city came to a standstill as taxi drivers, telephone operators and teachers lay ill. Garbage went uncollected, mail undelivered. When news got out that Franklin D. Roosevelt lay near death, it became clear that this disease ignored socioeconomic boundaries. Trying to allay the growing panic, the New York health commissioner, Royal Copeland, issued positive reports — “no reason for alarm” and “disease on wane.” Newspapers reported otherwise: 50,000 flu masks dispensed by the Red Cross, an acute nursing shortage, mansions converted into temporary hospitals.
Although the responsible microbe had not been identified, the New York City Health Department designed a control plan based on its experience with tuberculosis. This plan staggered business hours to diminish crowding on subways and elevated trains, suspended book circulation in public libraries and encouraged theaters to sell only half their tickets, leaving a seat empty between patrons. An amendment to the Sanitary Code directed people to cover their mouths when coughing and noses when sneezing; spitting became a misdemeanor. Despite these measures, death notices filled the newspapers. Pictures of stalwart-looking young men in uniform and glowing young brides in wedding gowns added poignancy to the printed words. On Oct. 12, in a defiant demonstration of patriotism, President Wilson and a crowd of 25,000 paraded down New York’s “Avenue of the Allies.” The next week, 2,100 New Yorkers succumbed to influenza.
Apprehension and grief pervaded the city. No one knew who harbored the influenza germ or who might fall ill; but everyone knew someone who had died. And there was no place to hide. Even if one had the means, leaving New York proved futile, since influenza was engulfing the country, terrorizing even the smallest towns. With no effective treatment, physicians felt helpless. This contagion was overwhelming the nursing force; many of the young and healthiest had already perished. If a visiting nurse was spotted on a street, a crowd surrounded her, begging for help. Desperate to ward off the illness, people wore camphor balls; others had their teeth extracted, believing they harbored the germs that caused influenza. Home remedies proliferated: red peppers, strychnine, whiskey, chloroform — all to no avail.
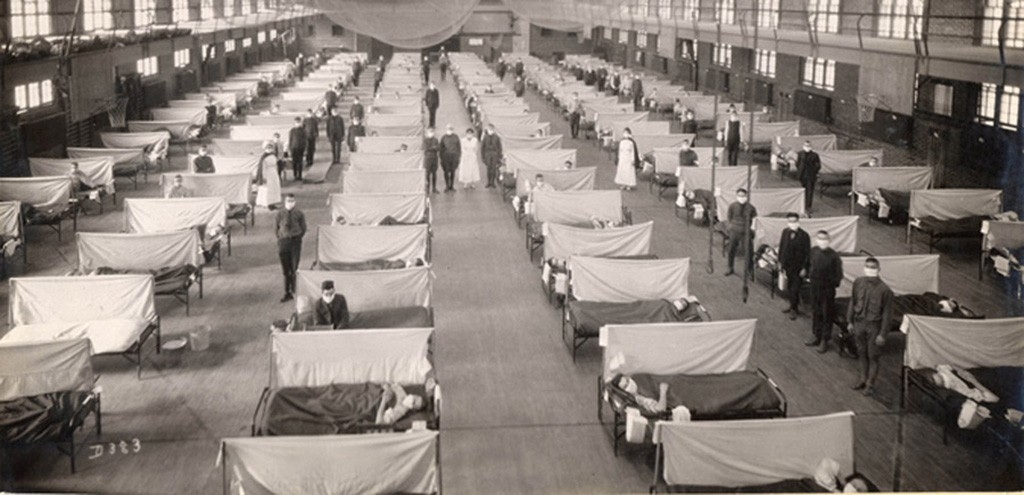
By the first week of November 1918, the death toll in New York reached 12,357. The deluge of patients swamped the wards and hallways of every hospital. Covered in white except for their eyes and hands, nurses resembled angels, or ghosts, moving through a sea of the ill — groaning, writhing, struggling to breathe. Photographs from the time reveal makeshift infirmaries set up in armories, gymnasiums and dance halls, with hundreds of cots lined up, each occupied by a body — some alive, some still. Obituaries listed entire families dead. The air reeked of decaying flesh as days passed before a death cart collected the deceased. Undertakers ran out of coffins; packed morgues closed their doors. Two thousand corpses lay unburied in Queens until sanitary workers came to assist the gravediggers. In desperation, some families buried their own. In a matter of months, an estimated 21,000 New York children became orphans.
Influenza traveled around the world with ferocity. Daily, the number of dead from the contagion almost equaled the tally of war casualties. The Nov. 11, 1918, celebration over Germany’s surrender was tempered by the scourge, which continued to stalk young adults worldwide. By the spring of 1919, the disease had run its course, killing more than 33,000 in New York, 850,000 in the United States, 20 million worldwide. And still no one knew what microbe had massacred a generation or how to prevent its horrifying return.
Born on Oct. 28, 1914, in East Harlem, Jonas Salk was just a child when these two plagues preyed upon New York. Spared, he would one day play a major role in the prevention of both. Salk’s work on the influenza vaccine would go largely unrecognized. His polio vaccine, however, would catapult him into a world of celebrity from which he could never extricate himself. When a waiting world learned on April 12, 1955, that his vaccine could prevent poliomyelitis, Salk, just 40 years old, became a hero overnight. Born in a New York tenement and humble in manner, he had all the makings of a 20th-century icon — a knight in a white coat. He had not anticipated the backlash from the scientific community, the one group whose adulation he craved. With the public awaiting his next medical triumph and his laurels tarnished by a cadre of academic naysayers, Jonas Salk had half a lifetime to prove himself.
