Good vibrations
Can Parkinson’s symptoms be stopped?
On June 17, 2018, Kanwarjit Bhutani stepped out of an elevator with his wife, unaware his life was about to change. A woman followed the couple from the elevator to the door of their condominium in New York City. Out of the blue, she recommended that Bhutani see Stanford Medicine researcher Peter Tass, MD, PhD, about his promising treatment for Parkinson’s — a vibrating glove.
Bhutani was still processing what had happened when he realized the mystery woman was gone. He had been diagnosed with Parkinson’s disease nearly a decade before, but only his close family and friends knew.
“I felt that Parkinson’s was something old people had. I don’t want to be associated with that. I’m not old, and I was very young — only 39 — when I got the disease,” he said.
For years he’d been managing Parkinson’s while juggling a career as president of several companies, including Tupperware U.S., Avon and Jeunesse. Then, the disease worsened without warning.
“All of a sudden, I couldn’t work,” Bhutani said. “I basically went into hiding.”
Bhutani scoured the internet for information on Tass’ research and introduced himself over email. Within minutes, Tass replied. In August 2018 Bhutani and his wife flew to the Stanford campus in Palo Alto, California, to meet Tass, who assessed Bhutani’s condition and explained the concept behind the glove.
“Most of it went over my head,” Bhutani said. “It was all la la land, to be honest with you. I didn’t understand much, but he said, ‘It’s noninvasive.’”
“It was noninvasive and it couldn’t hurt him,” added Bhutani’s wife, Suhkpreet Bhutani. “We had nothing to lose.”
Parkinson’s disease attacks brain cells that make dopamine, a chemical that is key to nerve communication for functions like movement, mood and behavior. Drugs that mimic dopamine are common treatments for the condition.
If the symptoms stop responding to drugs, deep brain stimulation is the gold standard treatment. The technique targets abnormal brain patterns with electrodes that are implanted into the brain and linked to a pacemaker-like device. Because of the risks of brain surgery, not all patients are eligible for or choose the treatment.
Yet, neither therapy is perfect. Drugs and deep brain stimulation are expensive and both can have serious side effects. They also don’t always work and, even when they do, their benefits can wane. So it might be hard to imagine that a vibrating glove could be much help.
But a recent study of a small group of patients found that wearing the glove for two hours, twice a day does just that, alleviating the tremor, stiffness, abnormal walking, slow body movement and balance problems associated with Parkinson’s.
Although the researchers didn’t set out to study other symptoms, they were surprised to find patients reported the glove also alleviated mood swings, behavior changes, depression and the loss of smell and taste.
“It seemed like magic,” said Stanford Medicine neurobiologist Bill Newsome, PhD, recalling the first time he saw videos showing improvements for Parkinson’s patients before and after using the glove.
“But Tass’ modeling studies suggest a plausible mechanism whereby fingertip stimulation could alter abnormally synchronous activity in the central nervous system.”
Convincing the research community the seemingly “magic” vibrating glove has real therapeutic effects will require further testing, explained Newsome, who holds the Harman Family Provostial Professorship and directs Stanford’s Wu Tsai Neurosciences Institute.
An old idea refined
The idea of using vibrations to treat Parkinson’s is not new, Tass explained. In the 19th century, neurologist Jean-Martin Charcot created a vibrating chair after learning that his patients’ symptoms briefly improved after long, jostling carriage and horseback rides.
Charcot’s vibrating chair, and the vibrating platforms and therapies developed by researchers who followed, alleviated some symptoms of Parkinson’s, but the results were inconclusive and temporary.
When Tass was a medical student, he became intrigued with self-organization — the seemingly spontaneous assembly of patterns and structures, such as clouds and snowflakes. He went on to earn a doctorate in physics and a master’s in mathematics for his research on self-organization, which revealed potential applications for neurological diseases, including Parkinson’s.
“My goal is to create treatments that are more effective and less brutal on the body by simply utilizing the self-organization power within the body,” Tass said.
How a buzzing glove could treat Parkinson’s
The symptoms of Parkinson’s arise when large groups of neurons abnormally fire in unison. Using computer simulations, Tass and his team discovered that a patterned stimulus that vibrates at a frequency of 100 to 300 hertz (cycles per second) can desynchronize neuron-firing. They called this coordinated reset stimulation.
Further, Tass discovered how to make the benefits of vibratory stimulus last, something that eluded Charcot and others who used vibrations to treat Parkinson’s: Pauses are crucial between treatments and within stimulus patterns.
The body needs to unlearn abnormal neural connectivity patterns, Tass explained. Just as taking small breaks increases the effectiveness of study or exercise, pauses improve the treatment’s effectiveness.
Tass explored possible therapeutic effects of the treatment by applying it directly to the brain with electrical stimuli via deep brain electrodes in studies in monkeys with Parkinson’s symptoms (Annals of Neurology, 2012) and later in a study of six Parkinson’s patients (Movement Disorders, 2014).
In the 2014 study in humans, coordinated reset stimulation was applied for three consecutive days in two daily sessions of up to two hours. The researchers found that the stimulation reduced the neural synchrony associated with Parkinson’s and this correlated with improvement of motor function.
“My goal is to create treatments that are more effective and less brutal on the body by simply utilizing the self-organization power within the body.”
Peter Tass, MD, PhD, professor or neurosurgery
Next, Tass and his team set out to find a way to deliver the stimulation without implanting electrodes in the brain. The solution was to replace electrical bursts delivered through electrodes embedded in the brain with vibratory bursts delivered through mechanical stimulators to the fingertips.
Fingertips have many sensory neurons, which means a large portion of the sensory cortex of the brain is dedicated to receiving signals from them. This is important because a noninvasive therapy must act on a sufficiently large portion of the brain to have similar benefits as deep brain stimulation. (This is also why fingertips are ideal for Braille, but not tattoos.)
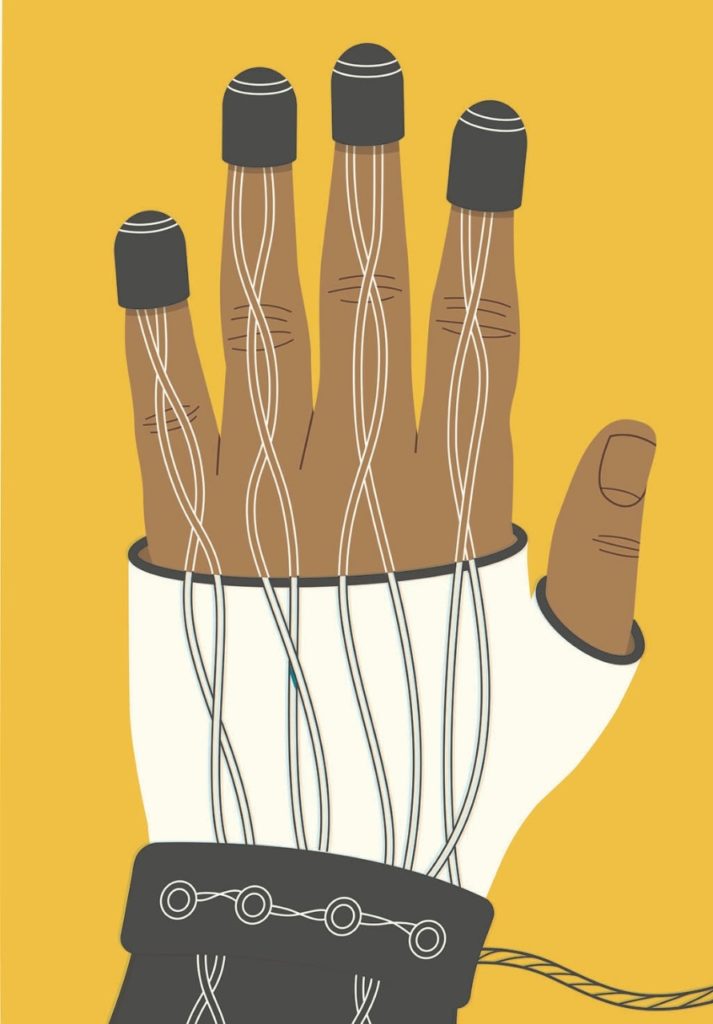
The outcome of this research is a strappy, skin-exposing glove that looks like something out of a sci-fi film. The glove is lightweight and can be worn while performing regular daily activities. It’s attached to a device that delivers bursts of 250 hertz (a buzz slightly stronger than a cat’s purr) through pin-sized openings on plastic pads strapped to the index, middle, ring and pinky fingertips.
Each glove collectively stimulates a patch of skin smaller than a dime.
What’s next for the research?
In April 2021, Tass and his team published the results of pilot studies of patients — including Bhutani — with mild to moderate Parkinson’s disease in Frontiers in Physiology. In these studies, eight Parkinson’s patients received vibrotactile coordinated reset stimulation daily for at least three months (three of those patients received the therapy for six or more months).
The researchers assessed patients’ motor function and obtained at-rest electroencephalographs before and after the three months of glove therapy using four subcategories — tremor, rigidity, bradykinesia (slow body movement) and axial (balance). They used EEGs, which measure brain activity, to investigate the therapy’s possible effects on the abnormal, synchronous neural patterns associated with Parkinson’s.
The researchers assessed the patients’ movements and brain activity off medication at the start of the study, at three months, and during follow-up visits approximately every three months thereafter.
These pilot studies revealed that the vibrations were well-tolerated, produced no side effects, improved the patient’s motor performance and reduced Parkinson-related neuronal synchrony in the brain.
“There’s currently no middle ground between drugs and invasive treatments for Parkinson’s patients,” said Leila Montaser Kouhsari, MD, PhD, a movement disorders neurologist at Stanford Medicine.
“Parkinson’s patients are often really suffering, but symptoms, such as tremor, can vary with stress and medication fluctuations, so they may not be ready to go all in with invasive procedures. Or, because of other health problems, they may not be able to get surgery,” said Montaser Kouhsari, clinical assistant professor of neurology and neurological sciences.
“Depending on how the clinical trial goes, the glove could expand what we have to offer patients. It could be huge if it helps a lot of patients with no side effects.”
For now, the glove treatment is available only to Parkinson’s patients participating in a clinical trial of the device that started Aug. 1. Tass is also working with an industry partner to gain U.S. Food and Drug Administration clearance for the treatment, which he hopes to have by summer 2023.
“Depending on how the clinical trial goes, the glove could expand what we have to offer patients. It could be huge if it helps a lot of patients with no side effects.”
Leila Montaser Kouhsari, MD, PhD, clinical assistant professor of neurology and neurological sciences
Newsome said the new trial is one of many important next steps: “The therapeutic effects need to be documented in a larger group of patients.” More research will be needed to identify which Parkinson’s patients are likely to benefit from the therapy, he said.
“Although much painstaking research remains to be done, this therapy is potentially game-changing because it is completely noninvasive,” Newsome said.
Before Bhutani used the glove as part of the study published this year in Frontiers, his Parkinson’s symptoms included muscle contractions, loss of taste and smell, inability to speak above a whisper, mood swings, and obsessive-compulsive buying behaviors. Each day he took 25 medications — some to treat Parkinson’s and others to alleviate the side effects of the other drugs.
At the beginning of his treatment, Bhutani wore the glove for two hours every morning, and two hours in the afternoon or evening.
Within three weeks, he said, his sense of taste and smell returned, and he was able to work in the garden again. Bhutani also reduced the drugs he was taking to 10 medications a day, and his muscles became less rigid and stiff, which restored his ability to show emotion with his face.
Bhutani still uses the vibrating glove, but not as often as he did initially because the benefits are lasting longer.
“In November 2018, I ran my first marathon,” Bhutani said. “It was a dream come true.”
His mood has also improved. “I feel my quality of life has come back. And I’ve got a very strong caregiver,” Bhutani said, smiling at his wife. “She has been by my side … I’m grateful to her.”
He’s also grateful to the mystery woman who suggested he contact Tass in the first place. Bhutani tried to discover her identity to thank her, but he never saw or heard from her again.
“I don’t know who she was, but she changed my life,” Bhutani said.
— For information about participating in a study of the glove’s effects, contact the Tass lab (https://med.stanford.edu/tass-lab.html) at parkinsonsvcr@stanford.edu.
— Contact author Holly Alyssa MacCormick for media inquiries at hollymac@stanford.edu.
— Watch a video showing the movements of a person with Parkinson’s’ disease before and after treatment with vibrotactile coordinated reset stimulation.
