‘We could be changing lives’
The importance of getting precise with mental health, treating it as health
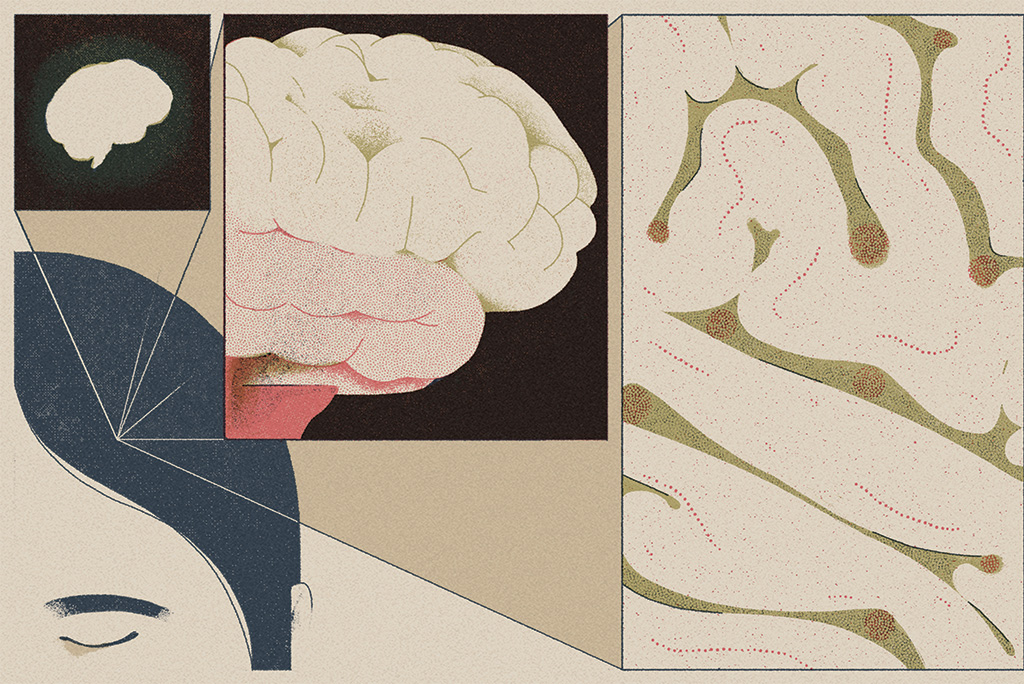
Imagine a world where, as a matter of course, your doctor asks you as much about your brain as your body. You talk about memory, mood and sleep. You go over family history of serious mental illness, neurodivergent disorders, depression and anxiety. And then your doc can order a detailed scan of your brain, called a functional MRI, to help map out its specific circuitry and look for signs of disruption.
Combined with details about your genetic makeup and responses you provide to specific questions or cues, it could help inform a personalized path for therapy. Which of the standard antidepressants are likely to be most effective? What regions of the brain are best to target with transcranial magnetic stimulation? Might one of the emerging psychedelic interventions play well with your circuitry — or a specific version of talk therapy?
Welcome to the world — still under construction — of precision mental health. It is a future envisioned and engineered by Stanford Medicine researchers, and it is fueled by the imperfect present where 1 in 5 U.S. adults deal with a mental health condition, yet only half of those seek treatment and roughly 30% of these patients experience no remission with any of the available treatments.
In a nutshell, precision mental health is the idea that measuring the biochemistry and circuitry of the brain, with all available tools and data, is as important as gathering evidence about the rest of the body — or more so given the high percentage of brain dysfunctions that can manifest life-threatening disorders. It is viewing what we now call mental health as brain health. Or, more succinctly, just health.
“There is such a sense of urgency with these conditions that if we could get this into practice, we could be changing lives.”
Leanne Williams, PhD, director of the Stanford Center for Precision Mental Health and Wellness
“There is such a sense of urgency with these conditions that if we could get this into practice, we could be changing lives,” said Leanne Williams, PhD, the inaugural Vincent V.C. Woo Professor of psychiatry and behavioral sciences. And perhaps saving them. Williams lost her partner, who suffered from untreated major depression, to suicide in 2015.
She and her Stanford Medicine colleagues at the Stanford Center for Precision Mental Health and Wellness, which Williams directs, are among a small segment of the psychiatry field aiming to show how this could work clinically. Though the medical establishment is slow to change, the movement is growing here and abroad, particularly in a post-pandemic world where recognition of mental health’s insufficient resourcing and one-size-fits-some approach is ubiquitous.
“For too long people have said, ‘The brain’s just too complicated.’ But we have enough of an understanding of brain architecture — of its main superhighways — to know what gets disrupted in all sorts of conditions,” said Williams, who recently secured her largest-ever grant, $18 million from the National Institute of Mental Health to study the cognitive biotype, a hard-to-treat type of depression her research team identified through brain imaging. “There is a clear consensus in the research world: ‘Why aren’t we moving this into the clinical world?’”
Imaging and biotyping
As Williams was beginning her career as a clinical psychologist in her native Australia, she recalls witnessing a patient diagnosed with schizophrenia hold a staticky transistor radio up to his ear, trying to blunt the voices in his head. “I thought to myself, ‘This is a circuit-level problem,’” she said.
Moments like that made her certain the clues to understanding psychiatric conditions lived in the world of neuroscience where the hows and whys of brain circuitry are investigated.
At the University of Sydney she helped establish one of the earliest labs connecting psychiatry and neuroscience. By the time she was recruited to Stanford, in 2012, she was convinced that brain circuitry’s contributions to psychiatric suffering were not trivial, nor was understanding that role out of reach.
“Leanne was determined this could be done — and she is showing the world how,” said Ruth O’Hara, PhD, senior associate dean for research, the Lowell W. and Josephine Q. Berry Professor of Psychiatry and Behavioral Sciences, and co-director of the Stanford Center for Precision Mental Health and Wellness.
Brain imaging is the primary tool used at the center. Functional magnetic resonance imaging has aided the identification of six large-scale circuits — those “superhighways.” Williams, O’Hara and colleagues have found that certain patterns of dysfunctions in these circuits — which they’ve named “biotypes” — correlate with specific variations of depression or anxiety and can help determine their best treatment options. Or at least rule some out.
“Depression is very heterogenous, yet we start with the same treatments for everyone.”
Laura Hack, MD, PhD, assistant professor of psychiatry and behavioral sciences and director of the Stanford Translational Precision Mental Health Clinic
A 2023 Williams-led study of 1,008 people with previously unmedicated depression, published in JAMA Network Open, found that individuals whose brain’s cognitive control circuit showed decreased activity in two particular regions were less likely than others to respond to traditional antidepressants.
The team labeled this group — which made up 27% of those in the study — the cognitive biotype. They are an example of the people who are likely to benefit from less commonly used medications or treatments like transcranial magnetic stimulation, or TMS.
When Williams’ partner died by suicide, she hadn’t yet associated specific quirks in neural circuits with specific symptom profiles. But she suspects now that his form of depression was consistent with the cognitive biotype, meaning he might have benefited from non-pharmacological treatments such as TMS.
“Depression is very heterogenous, yet we start with the same treatments for everyone,” said Laura Hack, MD, PhD, the lead author of the study, an assistant professor of psychiatry and behavioral sciences and director of the Stanford Translational Precision Mental Health Clinic, which puts Williams’ research into clinical use.
People with treatment-resistant forms of anxiety and depression who are referred there undergo a comprehensive battery of evaluations. The clinicians assess symptoms and neurocognitive ability, test blood for telltale proteins, analyze genetics to determine the ability to metabolize certain drugs, and look at functional MRI data gathered from patients at rest and while performing tasks. Patients and their referring doctors receive a report with a thorough explanation and the implications for treatment recommendations.
“In mental health, we have a tendency to move slowly to adopt our findings — unlike fields such as cardiology or oncology. This gives us a chance to speed things up in very important ways.”
Ruth O’Hara, PhD, co-director of the Stanford Center for Precision Mental Health and Wellness
So far, Stanford Medicine is among a small cadre of institutions around the world putting these methods into clinical use in psychiatry. Williams is also working with the U.S. Department of Veterans Affairs to apply precision techniques with vets who struggle with depression and PTSD. But she firmly believes primary care physicians of the future will also see these as essential tools for caring for their patients over a lifespan.
“I hear from many primary care providers who want this now,” Williams said. “It’s just a matter of making it available and getting them the proper training.”
Equally important, Williams believes, is making the unexplainable explainable to people suffering from little-understood — and therefore highly self-stigmatized — conditions. “When people can see, ‘Oh, this is what’s happening inside my brain,’ they can understand what’s making them ill, stop placing any blame on themselves and embrace treatment.”
Perhaps most importantly, the oftentimes agonizing gap between symptom onset and relief can be shrunk. “In mental health, we have a tendency to move slowly to adopt our findings — unlike fields such as cardiology or oncology,” O’Hara said. “This gives us a chance to speed things up in very important ways.”

