Ultrasound solution
A gentler way to shrink kids’ tumors
She’s only 5 years old, but after a summer of swimming lessons, Cadence May has mastered an impressive backstroke. She’s got the floating down pat, her mom says. She flutter-kicks with vigor. And she can stretch each arm way up behind her head, dig deep into the water of her neighborhood pool and propel herself smoothly along.
“I didn’t realize she would have full extension of her arm,” says Annette May, Cadence’s mother, recalling the moment she saw her daughter demonstrate her stroke for other students in swim class.
“She could do it flawlessly,” May says. “I was proud — and surprised.”
Watching Cadence master the backstroke was poignant for good reason: She was born with a desmoid tumor on her right forearm. Although these noncancerous tumors do not spread around the body, desmoids can grow aggressively at the site where they originate, leading to pain and permanent damage. Cadence’s tumor threatened to cause atrophy in her muscles and encase blood vessels and nerves, which could have seriously impaired movement of her arm and hand. When her doctor diagnosed the tumor in 2014, treatment options for children were bleak.
But instead of sustaining permanent damage to her arm, this young girl had an unusual opportunity to become a medical pioneer. In an April 2016 procedure at Stanford, when she was 3, Cadence became the youngest child in the world to be treated — for any disease — with a technology called high-intensity focused ultrasound. Today, her tumor isn’t completely gone, but it’s also not bothering her, and her doctors are using focused ultrasound to keep it that way.
Children with other diseases stand to benefit, too. Though the ultrasound technique helping Cadence has been used to treat a handful of conditions in adults for more than a decade, it’s undergoing a renaissance that promises to be especially advantageous for kids.
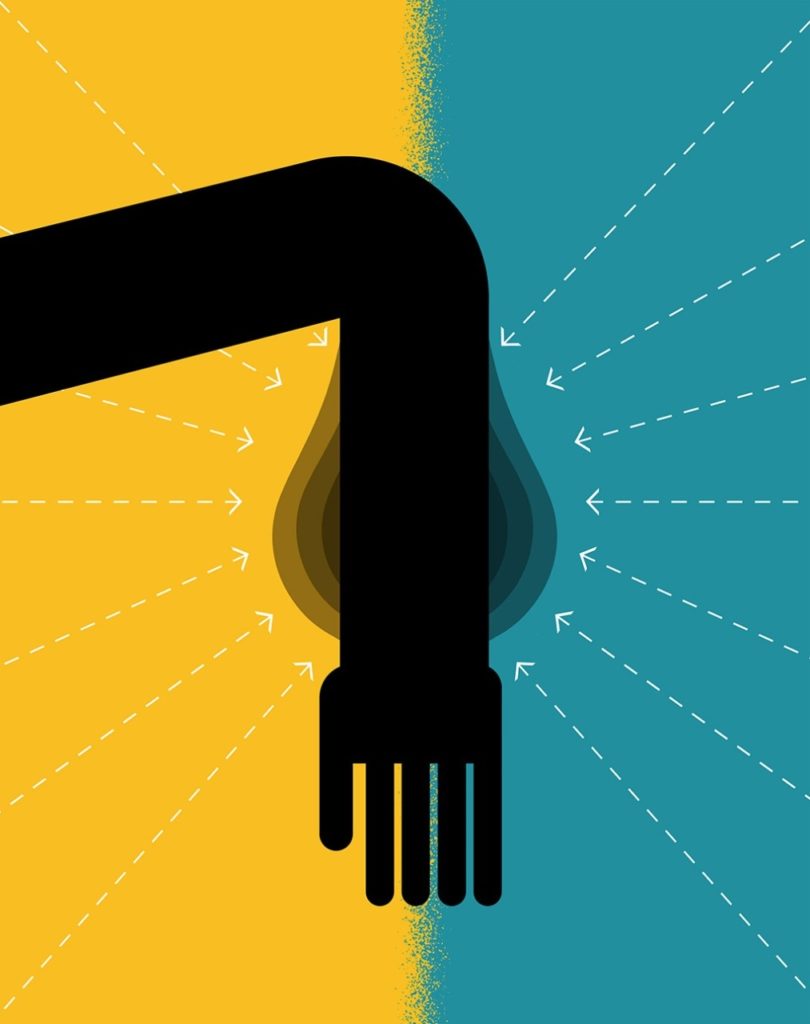
Focusing the beam
The idea behind focused ultrasound is simple: Instead of projecting high-frequency, impossible-to-hear sound waves diffusely through tissue, as doctors do during ultrasound imaging, they focus the sound waves on a single location to heat and kill only a region of problematic tissue. The waves originate from a transducer, traveling through healthy tissue in a cone shape and cooking only what’s located at the tip of the cone of energy. The procedure is done in a magnetic resonance imaging scanner to help doctors direct the high dose of energy to just the right spot.
“It’s like taking a magnifying lens to focus sunlight and burn a hole in a leaf,” says Pejman Ghanouni, MD, PhD, assistant professor of radiology at Stanford, who used the technology to treat Cadence. “The tissue at the focus is heated and destroyed. We use MRI to image what we’re going to target, and also to monitor the heating. We try to ensure that the target is adequately heated while avoiding damage to the surrounding tissues.”
The ultrasound transducer delivers several zaps of energy, each lasting 20 to 30 seconds, throughout the targeted area. (Some physicians use ultrasound imaging to guide focused ultrasound treatment, but this does not allow monitoring of how much the tissue heats up.)
“It’s completely noninvasive, doesn’t require a knife, and you can reach inside the body and destroy tissue in a region as small as a grain of rice,” says James Geller, MD, a pediatric oncologist at Cincinnati Children’s Hospital who referred Cadence to Stanford. Geller’s team is now launching a focused ultrasound program of its own, one of about half a dozen such programs treating kids across North America.
Focused ultrasound was first approved by the U.S. Food and Drug Administration to treat uterine fibroids; it also has approval for relieving pain from cancerous tumors that spread into bone and treating essential tremor. Nearby tissues are sometimes overheated, with sunburnlike burns or blisters possible if the targeted area is near the skin, though physicians are developing methods for using water cooling to reduce this risk. After the problem area is heated and killed, the body gradually absorbs the dead tissue.
Focused ultrasound is especially promising for treating growths that cause damage in the areas where they appear but don’t spread around the body.
Ghanouni and other experts think the advantages of focused ultrasound justify expanding its uses much further. The technique is especially promising for growths that cause damage in the areas where they appear but don’t spread around the body, such as desmoids, certain bone abnormalities, benign brain tumors and other neurologic defects. For locally aggressive but noncancerous tumors like desmoids, using high-intensity focused ultrasound requires doctors to shift their thinking from permanently vanquishing a tumor to controlling it — but it also offers distinct advantages in terms of speed and safety.
“The idea of being able to put a child in an MRI scanner and have their lump treated when they come out sounds almost 22nd-century,” Geller says.
A persistent lump
When Cadence was born in 2012, her parents wondered what was wrong with her arm. “We initially noticed what looked like trauma to her right arm,” says Aaron May, Cadence’s father. “It just looked swollen. We kind of joked that it looked like a Popeye forearm because it was noticeably larger than the other one.”
Physicians in the family’s hometown of Louisville, Kentucky, said the lump would disappear on its own. When it didn’t, the Mays requested a referral to Cincinnati Children’s, where, in June 2014, Geller’s team diagnosed a desmoid tumor. These rare tumors occur in 900 to 1,000 people in all age groups nationwide each year.
“Desmoids are unique because they’re not cancer; people don’t die from them, but people are tortured by them,” says Raffi Avedian, MD, assistant professor of orthopedic surgery at Stanford, who helped treat Cadence.
The tumors infiltrate muscles and cause pain and deformity, he explains, and traditional cancer-fighting techniques often fail. “People get all the side effects of radiation, chemo and surgical scars, and a lot of times the tumor comes back,” Avedian says. “There’s all that effort for really no benefit.”
For Cadence, Geller initially suggested a year of chemotherapy, a then-common approach. Cadence, who had just turned 2, had a port inserted under the skin of her chest to enable weekly intravenous chemo infusions.
Although she didn’t have serious side effects from the drugs, the weekly two-hour drives between Louisville and Cincinnati were draining for the whole May family. And Cadence’s port had to be accessed with a needle inserted through her skin each week, which she hated. She received numbing cream before each treatment, but could still feel the needle. Often, four to six people had to hold her down so her nurse had the best chance of hitting the port on the first try.
“It was pretty painful, watching her scream in pain week after week for 26 weeks,” her mom says. After six months of chemotherapy, the desmoid had grown slightly. Feeling discouraged, Cadence’s parents ended the infusions. Ten days of oral chemotherapy — with the side effect of a rash so severe it landed her in the ICU — was equally disheartening, so the family stopped Cadence’s treatment completely. She continued receiving MRI scans for monitoring; in early 2016, after nine months without medication, the tumor had grown more. That’s when Geller referred the Mays to Stanford, where Ghanouni’s team offered to treat Cadence. The Stanford physicians had been studying focused ultrasound for other diseases and had recently gained permission to offer it to desmoid patients on a compassionate-use basis.
Avoiding overkill
Hearing about focused ultrasound gave the Mays their first real hope. “It was less invasive, it wasn’t going to be painful and she wasn’t going to have to be cut open,” Aaron May says. The couple had already heard that surgery was a poor option.
“Even after resections where the pathologist reports that the margins are clean, there’s still a 50 percent chance that a desmoid will come back,” Ghanouni says. “Our surgeons aren’t excited about operating on these tumors.”
If focused ultrasound hadn’t existed, Stanford’s team could have offered Cadence surgery, albeit with large risks. “The expected side effects would have been related to removing muscles and nerves, leaving her with significant functional loss of her arm,” says Avedian. That would have been the best-case outcome: Before focused ultrasound was introduced, Avedian sometimes had to amputate limbs of children who had aggressive returning desmoids.
Radiation, which is a good option for many adults with desmoids, is less likely to resolve pediatric desmoids and carries higher risks for kids. “If you expose a child to radiation, you also give them a 1-in-20 chance in their lifetime of developing an actual sarcoma, a malignant tumor,” Ghanouni says. For an older adult, in whom the radiation is more likely to be effective, that 1-in-20 risk may seem more acceptable.
“But the risk-to-benefit relationship is very different in children,” Ghanouni says, noting that kids also have many decades of remaining life expectancy in which a secondary cancer caused by radiation could appear. “Kids are not small adults, so we really need different treatment options.”
‘Nerve-wracking’ procedure
Shortly after 8 a.m. on April 14, 2016, Cadence was put under general anesthesia at Lucile Packard Children’s Hospital Stanford, then wheeled to Stanford Hospital and positioned on the MR-guided focused ultrasound table. Although the focused ultrasound equipment is located at Stanford’s adult hospital, a pediatric anesthesia team from Packard Children’s collaborated with Ghanouni throughout the procedure to keep Cadence safe. (Packard Children’s new hospital, opening in December, will have focused ultrasound equipment dedicated to pediatric patients.)
“These tumors are in the water spaces, the ventricles, in the brain. They can grow and obstruct the brain’s plumbing.”
“It was nerve-wracking treating someone so young,” Ghanouni says. The technology had been used for a few desmoid tumors in adults, and Ghanouni and Avedian had collaborated on five desmoid cases in teenagers, making them the first U.S. physicians to use it to treat pediatric patients.
In Cadence’s case, the team’s main concern was to protect her skin, nerves and bone. Ghanouni planned to limit the ultrasound treatment to the tumor’s core, aiming to kill 30 percent of it. When Avedian met with the Mays, he used MRI images to show where the high-energy beams would go.
“We were taken aback a little,” Aaron May says, recalling when the couple first heard the plan. They had hoped physicians could eradicate all of Cadence’s tumor, yet understood the need for caution.
During the procedure, Ghanouni and his colleagues spent nine hours zapping the middle of the lump bit by bit. At the end, they were confident the tumor’s core was dead. “He did what he said he was going to do, and he told us this is not a one-time treatment, that he could go a little further each time,” May says. Indeed, a major advantage of focused ultrasound is that, unlike toxic chemotherapy or DNA-altering radiation, there is no limit to the number of treatments a patient can receive.
Cadence stayed overnight at Packard Children’s for monitoring as the anesthesia wore off, and was her usual self soon after. “The very next day, she was playing on the playground like nothing had ever happened,” Annette May says. That day Cadence had no trouble swinging from the monkey bars using both arms, her mom says.
Seeing how quickly Cadence bounced back increased the confidence Ghanouni and Avedian had in what they were doing. “What we’re learning from desmoids can translate to sarcomas and other tumors as well,” Ghanouni says.
Treating other tumors
Avedian, Ghanouni and their Stanford colleagues are continuing to study how focused ultrasound could be used against several types of tumor. They have conducted a clinical trial for patients with malignant sarcomas — cancerous soft-tissue and bone tumors — and have used focused ultrasound to treat benign bone tumors called osteoid osteomas, as well as vascular malformations, which are overgrowths of blood vessels. For all of these diseases, existing therapies have drawbacks that the Stanford team thinks focused ultrasound may be able to circumvent. In sarcoma treatment, for instance, recent advances in radiation, chemotherapy and surgery haven’t improved patient survival; the scientists hope folding focused ultrasound into the mix will yield better results for patients in the long run.
A major impediment to using focused ultrasound more widely is that, with the exception of the small number of FDA-approved applications, insurance doesn’t routinely cover it. Fighting for insurance authorization, sometimes through several rounds of appeals, can be time-consuming. Although some children are now treated through clinical trials, finding patients who are good candidates for research and are willing to participate can be a slow process.
“It’s also technically challenging,” Ghanouni adds. The team giving the treatment needs to understand the complex physics of ultrasound — how to blast sound waves from several different points of origin so that they converge, in phase, on the problem tissue — as well as how to correctly monitor the procedure with MRI, the medical details of each condition being treated and how to provide appropriate anesthesia for many types of patients. Bringing all these areas of knowledge together requires the expertise of a place like Stanford.
“It’s not plug-and-play,” Ghanouni says. “Frankly, focused ultrasound has needed some champions.”
Challenge of brain tumors
The brain, however, is the most challenging frontier. The thick, uneven skull bone sends sound waves off target, so radiologists must have a detailed CT scan of the patient’s skull to figure out how to compensate for deflections caused by its topography. An additional complication is that sound waves travel through bone 20 times less efficiently than through soft tissue, heating the bone as they traverse it. Before the therapy, patients must have their heads shaved to prevent trapping air bubbles near the bone that further exacerbate sound wave deflection; they must also wear a cap filled with chilled water during treatment to keep the skull evenly cooled.
These problems have been addressed in adults — who can receive focused ultrasound for such diagnoses as essential tremor and Parkinsonian tremor — and now researchers want to bring the potential benefits to children with neurological conditions. Ghanouni and Stanford neurosurgeon Gerald Grant, MD, are collaborating with others at Nicklaus Children’s Hospital in Miami to conduct a trial for children with tuberous sclerosis, an inherited disease that causes tumors in many organs. Some patients develop benign brain tumors called subependymal giant cell astrocytomas, or SEGAs.
“These tumors are in the water spaces, the ventricles, in the brain. They can grow and obstruct the brain’s plumbing,” says Grant, associate professor of neurosurgery at the School of Medicine and division chief of pediatric neurosurgery at Packard Children’s. The tumors are operable, but treating them surgically requires cutting through healthy structures to reach them. Depending on the exact size and location of the SEGA, a child’s memory tracts may be damaged, or the corpus callosum, which connects the two halves of the brain, may have to be severed. Recovery from surgery takes three to six weeks, and the surgery increases the patient’s risk of seizures later on.
Against that background of risks for more accepted treatment methods, focused ultrasound is appealing. Because SEGAs are benign, controlling but not completely eradicating the tumor may be acceptable. In addition, SEGAs have well-defined edges on MRI scans and few blood vessels, characteristics that make them a good fit for treatment with focused ultrasound.
Cancerous brain tumors are more challenging targets. They tend to have long fingers that infiltrate healthy brain tissue and are fed by many blood vessels. These blood vessels create a hazard for focused ultrasound because accidentally severing one could create a deeply buried brain hemorrhage that would be hard to control.
But there may still be a role for focused ultrasound in brain cancer treatment; scientists at other institutions are experimenting with using it to temporarily open the blood-brain barrier to let chemotherapy drugs enter the brain. The Stanford team also has plans to conduct trials of this technique. Some teams have also packaged chemo drugs inside liposomes (bubbles of fat) that could be melted with focused ultrasound to release drugs where they’re needed and minimize side effects elsewhere in the body. The technique is promising for tumors growing inside and outside the brain.
In the meantime, Grant and his collaborators will proceed cautiously in testing whether focused ultrasound can help kids with SEGAs. They’ll look for patients who would otherwise require invasive surgeries and whose imaging scans show tumors the technique could safely hit.
“We’ll advocate for trying this because, in the right cases, where it is safe and could improve the child’s quality of life, we wouldn’t feel like we would have much to lose,” Grant says.
A happy kindergartner
Cadence’s outcome is promising. Late last year, her desmoid grew again — it had been about 15 ml in volume after the first treatment, but expanded to 24 ml — so she returned to Stanford for a second focused ultrasound treatment in December. The entire trip took four days, and Cadence was making snow angels and sledding with family soon after.
Ghanouni plans to keep zapping the center of the lesion as needed to prevent it from interfering with Cadence’s life. In addition to the teenagers treated before Cadence, Ghanouni has also treated 32 adults with desmoids and says other patients have begun to seek him out after reading about the Stanford team’s early results in online support groups.
For the long term, Ghanouni hopes another scientist will develop a treatment that vanquishes desmoids for good. “There are some exciting drugs on the horizon with promising results for desmoids,” he says. The longer he can help children like Cadence avoid amputations, radiation and chemotherapy, the more options they will have later, he adds. “Focused ultrasound doesn’t burn any bridges for these kids.”
Today, Cadence is a happy kindergartener who is excited by Ghanouni’s “magic tools” but who otherwise doesn’t mention her desmoid much. To her, it’s just part of her arm.
“This summer, another girl at swim lessons asked, ‘What’s that on your arm?’” her mom recalls:
“It’s my bump,” Cadence told her.
“How did you get it?” the other child asked.
“I was born with it,” Cadence said. Then, after a minute, she added, “I don’t want to talk about it anymore.” “OK,” said the other girl.
Then they jumped into the water, two little girls at any swimming lesson anywhere. They floated. They kicked. They stretched their arms above their heads, dug into the water, and learned how to swim the backstroke.

