Unsheltered
Inside a clinic for homeless people in Silicon Valley's birthplace

Every Monday, Crystal Unzueta, MD, a family medicine physician and clinical assistant professor who recently joined Stanford Health Care, works at a small Palo Alto clinic a five-minute drive from Stanford University’s campus.
Her “most frequent patient,” a 62-year-old man with poorly controlled diabetes, usually drops in on Monday mornings to have his pill box refilled. Mr. Issac, as Unzueta calls him, has been homeless for many years and doesn’t want to risk carrying around all his medications.
Peninsula Healthcare Connection provides free health care to people like Mr. Issac who are homeless or at risk of becoming homeless. It’s staffed by physicians from Stanford Health Care and the Palo Alto Medical Foundation who take shifts a few times a month. Unzueta is from a Mexican American family and has spent the early years of her career working with lower-income, Spanish-speaking communities. In fact, it was the opportunity to work at a clinic like this that convinced her to move to Stanford Health Care.
Patients come to Peninsula Healthcare Connection with the same complaints as patients in any other clinic: diabetes, high blood pressure, allergies, sleep problems, stress from the slings and arrows of modern life. They come in to refill their prescriptions, to get their flu and COVID-19 vaccines, to seek help quitting an addiction, or to get a rash checked out.

But the fact that a large proportion of the clinic’s patients have no home address stacks the odds against them. Some have been unhoused for decades. They live on the streets, in tents, in their cars, or move from one temporary shelter to another. Their lack of housing can exacerbate their health conditions, limit their access to care, and hinder their ability to make healthy choices.
Mr. Issac’s diabetes is so poorly managed that it’s put him in the hospital several times. “The first time I saw him he had just been released from the hospital. He was there because his sugar level was so high it was unreadable in clinic,” Unzueta said. Having high blood sugar affects not only his physical health but also his mental state, often leaving him confused.
“It’s really difficult for you to check your sugars when what’s on your mind is, ‘Where am I going to sleep tonight?’ you know?” Unzueta said.
Recently, he had tried staying in a shelter recommended by clinic staff but left because of a loud snorer. He told Unzueta that he’d rather sleep outside by the train tracks.
The basic requirements of managing his diabetes — eating a low-carbohydrate diet, taking his pills and having insulin shots with regular meals — are often impossible for Mr. Issac to manage.
He needs insulin shots twice a day, but the insulin needs to be kept in a refrigerator, which he doesn’t have, though he tries his best by keeping it with an ice pack. Some nights he has dinner, some nights he has no food. When he can find a free breakfast program, it’s usually pancakes or something similarly high in carbohydrates.
For the doctors who staff the clinic, the work can be rewarding and, for some, a reminder of why they went into medicine. They can make a real difference in their patients’ lives and yet, as physicians, they cannot change the stark reality of their patients’ homelessness, which often comes with broken social ties and past traumas. With no guarantee of shelter, food and safety, staying healthy is next to impossible.
Nowhere is it more clear that health is determined by more than medical care.
According to a 2022 survey, more than 10,000 people are experiencing homelessness in Santa Clara County, which bills itself as the “birthplace of Silicon Valley.” Peninsula Healthcare Connection, located in the north end of the county, serves around 4,000 people a year, mostly from Palo Alto or East Palo Alto.
The clinic — two exam rooms, a tiny office and a chair in the entryway that serves as the waiting room — is part of the Opportunity Center, a nonprofit program that provides permanent housing and services to previously unhoused people. Founded in 2006, the clinic is largely supported by federal and local grants, including funding through Stanford Health Care’s Community Partnership Program.
For the doctors who staff the clinic, the work can be rewarding and, for some, a reminder of why they went into medicine.
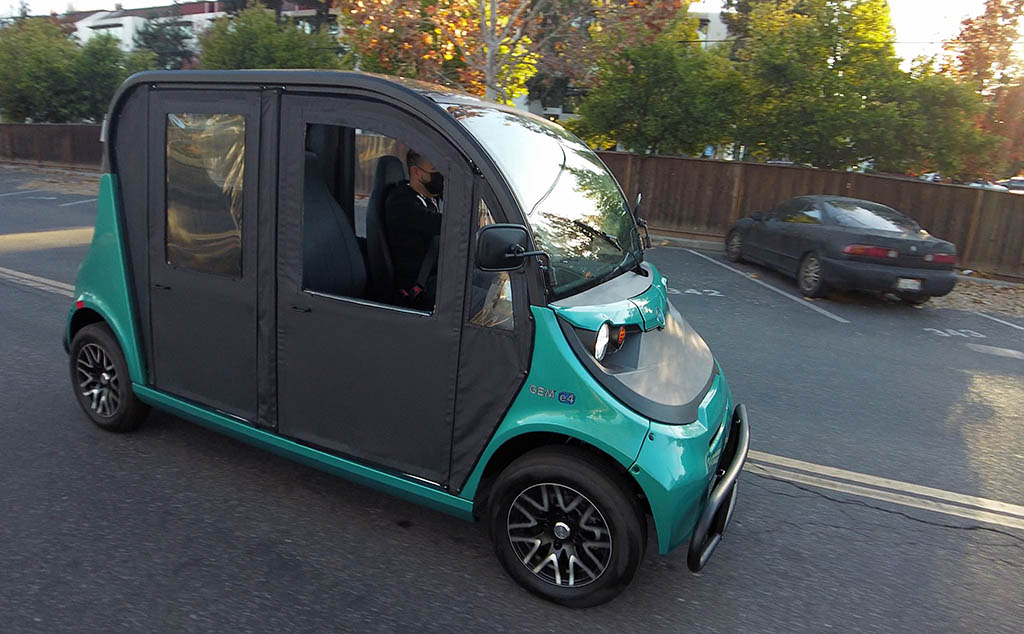
Recently, a grant from Stanford Health Care allowed the clinic to purchase an outreach vehicle — a sort of semi-enclosed, street-legal golf cart — which will help address a common barrier for homeless patients: transportation.
“It’s a game changer,” said Drew Navarro, the clinic manager and designated driver of the new vehicle. Many patients take multiple buses and trains to get to their appointments and even those with cars may not be able to afford gas. Having the new vehicle will enable Navarro to bring patients to the clinic, to a hospital appointment, or pick them up from the train station.
Navarro leads the clinic’s outreach efforts, which include a street medicine team that goes out to encampments twice a month. The team is equipped to treat wounds, give out antibiotics, take blood pressure and blood sugar measurements, or even collect urine samples to take back to the clinic. “The whole point is to meet them where they are, because we know not everyone’s going to come into a clinic,” Navarro said.
He and outreach worker Michelle Myers are the familiar faces that can finally convince someone to get care at the clinic. They even do a bit of matchmaking between patient and physician to find the best fit.
“Drew and Michelle are really the heroes. They’re the ones that really know the patients and the ones bringing folks in,” said David Shi-Ann Chang, MD, an internist and clinical assistant professor who oversees the group of Stanford Health Care physicians at the clinic.
At 10 o’clock on a warm Monday morning in November, the clinic was quiet. Unzueta checked her schedule for the day. She had only three appointments on the books, but Mr. Issac usually drops in without one.
The previous Monday, Mr. Issac showed up at the clinic feeling dizzy and looking extremely pale. His sugar levels were in the 500s — three times the normal level — so the clinic had to send him to the emergency room again. Unzueta wondered how he’s doing this week.
The first patient on this day arrived for his appointment at 10:30 a.m. José, 59, is tall and has close-cropped, salt-and-pepper hair. He’s there because his urine smells bad. Unzueta spoke with José in Spanish, his preferred language. This was his first visit with Unzueta, and he’s animated and talkative.
He tells her he has bipolar disorder, which makes him hallucinate voices and sinks him into depression most of the time. On Tuesdays, Wednesdays and Thursdays, he cares for and stays with his elderly mother, who has dementia. His siblings, worried about his bipolar disorder, won’t let him be more involved. That means Mondays, Fridays and weekends, he’s out of luck.
Families, Unzueta said, often don’t know how to deal with mental illness in their loved ones.
Because José is considered partially housed, he doesn’t qualify for a place in a long-term shelter. Four days a week, he sleeps in a tent on the street, where he’s had his medications stolen, gotten into fights and been harassed by police.
It’s a difficult, depressing life out there, he told Unzueta, holding his head in his hands, but he’s determined to stay as healthy as possible so he can take care of his mother.
Unzueta spent about 45 minutes with José, talking over his concerns, his medical history and his living circumstances. She examined him and gave him a referral to a urologist at Stanford Health Care. Before he left, she also set him up to get a COVID-19 booster shot.
“Unless a clinic is set up with doctors and staff who understand that you need a lot of social services and wraparound support for these patients, it’s not well equipped to take care of them.”
David Shi-Ann Chang, MD, who oversees Stanford Health Care physicians at the Peninsula Healthcare Connection clinic
Relatively long visits like this one are the norm at Peninsula Healthcare Connection, but a rarity in primary care clinics where patients are often filed in and out in 15 minutes. The slower pace allows physicians to build trust with their patients and learn about nonmedical circumstances — like housing, food and employment — that can affect their health.
“They don’t teach you this in medical school,” Unzueta said about accounting for the challenges of homelessness for her patients. She’s worked a lot with low-income communities before, but never with so many patients without housing. “Five years out of residency and I’m only now learning how a homeless shelter works,” she said.
The truth is, not all physicians want to work with the homeless population. “There’s still stigma associated with taking care of patients who are unhoused,” Chang said. “Unless a clinic is set up with doctors and staff who understand that you need a lot of social services and wraparound support for these patients, it’s not well equipped to take care of them.”
Chang grew up in Palo Alto, known for its affluence. His homeless patients include former software engineers and a high school classmate. Working at the clinic has opened his eyes to how easily someone can lose their housing.
“It’s sobering and also humbling to think all these environmental forces could have pushed anyone, really, onto this different pathway,” he said.
Though most of the patients at Peninsula Healthcare Connection have a case worker from the Opportunity Center to help connect them with social services, the physicians often find themselves in the role of patient advocate.
Angie Chen, MD, is a Stanford Health Care addiction specialist and clinical associate professor who works at the clinic every other Tuesday.
“Everybody is an amazing case of hope and effort and tragedy,” Chen said of her patients.
Maggie, in her 50s, for example, had a thriving career in advertising before she became homeless in 2018. She takes buprenorphine for an opioid use disorder and Adderall for attention-deficit/hyperactivity disorder. After her psychiatrist died in November 2021, she found her way to the clinic, where she sees a psychiatrist and Chen.
When Chen learned that Maggie was paying $400 a month for medications she should have been getting for free, she called the pharmacy and told them that the drug costs were now covered by Medi-Cal, California’s Medicaid program. Such oversights are not uncommon and can be the deciding factor in someone’s ability to stay healthy. “Most pharmacists have no idea,” Chen said.
Another of Chen’s patients, Charles, is trying to quit drinking, but at a visit in October, he was panicked about a problem with his Social Security payments. Chen found him some information for a pro bono lawyer.
“It’s common for us to see folks whose ties with family have been severed for whatever reason. They don’t have a life raft to help them through harder times. They have nowhere to go and nowhere to turn.”
Laura Vaughan, MD, a Stanford Health Care physician who works at the clinic
The stress of losing steady income made him want to drink, he said, and staying sober had been that much harder. He was anxious and irritable. Nevertheless, he hadn’t had a drink since the last time he saw Chen two weeks earlier. “It’s a conscious effort. I appreciate that so much,” Chen told him, giving him a fist bump.
Charles is 62 and had his first drink at age 6. His mother was an alcoholic, and he’s estranged from his wife and kids. He didn’t like staying in a shelter because he couldn’t stand being around other people. He asked Chen if it was bad for him to be alone all the time. She told him about a study in which rats were given a choice between getting an addictive drug like heroin or playing with other rats. They chose the latter. Like the rats, “we are social creatures,” said Chen.
For people who are homeless, a social support network is hard to find. Sometimes it’s a matter of choosing between a housing opportunity that takes them away from the community they’ve managed to make or staying and living on the streets.
“People and relationships are essential to human health,” said Laura Vaughan, MD, another Stanford Health Care physician who works at Peninsula Healthcare Connection. “It’s common for us to see folks whose ties with family have been severed for whatever reason. They don’t have a life raft to help them through harder times. They have nowhere to go and nowhere to turn.”
“We provide the medical piece, but the social piece is really what matters, and that’s harder,” said Vaughan, an internist and clinical assistant professor.
She sees it as part of her job to work with the case workers to figure out where medical care falls in a patient’s hierarchy of needs. Oftentimes, social needs — like housing or transportation — are higher on their priority list than taking their blood pressure medication.
When Unzueta prescribes medications for her patients who have no housing, she keeps in mind that it may be the last time she’ll see them. She’ll choose the medication that has the least risk of side effects, for example. Lately, she’d considered switching Mr. Issac to a new type of insulin that is administered only once a week.
“Yes, he needs insulin because everything is just so uncontrolled. But it’s not really practical for him, it’s not really feasible,” she said.
Mr. Issac didn’t show up at the clinic that week. “You kind of always think, this patient may not be able to come back,” Unzueta said. But the next Monday, he returned. And he came in with an empty pill box — a good sign that he’d remembered to take his medications.

