In the fog of loss
A reflection on love, life and death
The first symptoms announced themselves with stunning swiftness: back pain, gut pain, a dramatic darkening in the color of my husband’s urine. Jim was 62 years old, a lifelong runner, in great shape. Handsome, funny, smart, and crazy about me, as I was about him. Just the week before, he’d brought our bicycles to the shop to be tuned up in preparation for a 100-mile ride. Now he lay flat on the couch, his silence more alarming to me than groaning might have been.
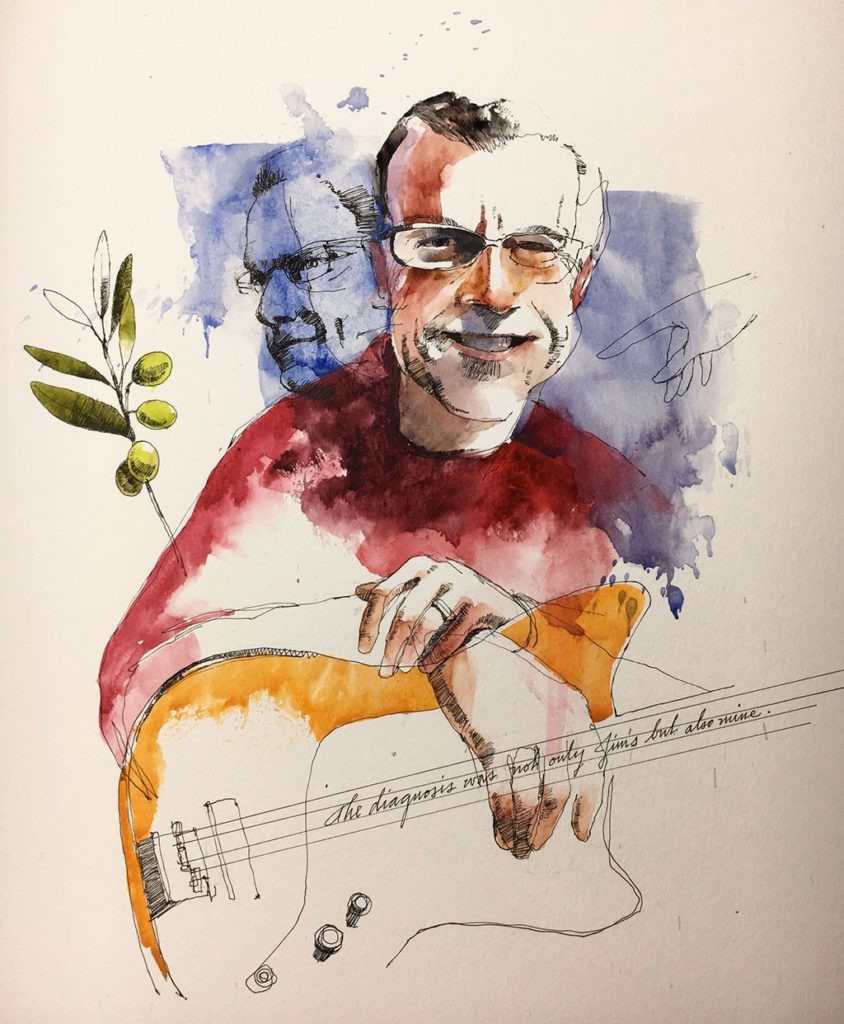
Just 15 months had passed since our wedding — a second marriage for us both, on a New Hampshire hillside near where I came from, with 100 friends and the six grown children from our long-ago first marriages gathered around, as the two of us held hands and spoke of the great adventure that lay before us. Whatever the actuarial tables might have told us about our prospects, we envisioned many good years ahead. How lucky, everyone said, that we had found each other when we did. He called me his Brigitte Bardot. I called him my guard dog.
The following spring we bought a house in the Bay Area and staked out a spot for planting olive trees. First harvest five years down the road, but we were patient.
Then this. “Do I look a little yellow to you?” He did.
What the doctor said
The pain arrived like a thief in the night, and by the following day it was bad enough that we went to the hospital for scans. As we sat in the doctor’s office waiting, a feeling of dread came over me. When the doctor entered the room, I knew it was bad.
“We can’t confirm this until we perform the endoscopy,” he told Jim, “but it’s pretty clear what’s going on here. There’s a tumor in your pancreas.”
I looked at Jim’s hands, his shoulders — stiffening, his beautiful thick hair (the envy of our balding friends), his dear, lined face. He still looked like himself, but everything was different now, life as we’d known it gone in the space it took for a man we’d never met to deliver that one sentence.
Now this man was putting his hand on Jim’s shoulder.
“I’m so sorry,” he said. “My father died of this.” Emphasis on the word “father” with the implication clear: and you will too.
There was more, though I could take in only part of it, words coming in and out like bad radio reception. The tumor appeared to be 2.5 centimeters in diameter. The good news, if you could call anything good now, was that the cancer appeared to be what is known as “locally advanced,” meaning that it had not spread to other organs. Not yet. The term for this tumor was “borderline resectable,” the prospects for surgically removing it slim. Without surgery, Jim was likely to die within a matter of months. A year at most, probably.
In the space of a moment, I had a strange new definition for what constituted good luck.
I looked again at my husband. My husband — a word I had not uttered for 24 years, until I spoke my vows to Jim. For 24 years I’d lived as a solo operator, but not anymore. The diagnosis was not only Jim’s but also mine.
His face conveyed little. I touched his shoulder, drew in my breath.
“And what happens if Jim gets this surgery?” I asked. Because he had to. There was no other acceptable option.
The doctor laid it out for us. The surgery a person needed in a situation like Jim’s — the only route to surviving cancer of the pancreas — was known as the Whipple procedure. One of the most involved of all surgeries, it called for the removal of part of the pancreas, the gallbladder, the duodenum, as well as every lymph node the surgeon could get his scalpel on, and a complete rerouting of the digestive system. This was an enormously painful, life-altering procedure. Only a small percentage of those diagnosed with pancreatic cancer would qualify to undergo the Whipple. And even for those able to undergo the surgery, 80 percent would experience a recurrence, often within the first couple of years.
In the space of a moment, I had a strange new definition for what constituted good luck. Good luck meant that we got to hold onto some small shred of hope, and hope required the Whipple procedure.
I don’t remember how we got down the hall to the elevator, and from there to the parking garage, though I know Jim drove us home.
A new way of life together
Next morning, I began my research into our alternatives. A physician friend sent me links to papers not generally available to the layperson on new research into pancreatic cancer — immunotherapy, gene therapy, proton therapy. Bent over our kitchen table late into the night, or before dawn, I struggled to make sense of them. I spent my days on the phone with three yellow legal pads in front of me and a separate receiver on each ear, so I could speak with one medical facility while on hold at another — getting up at 5 a.m. to start placing calls to the East Coast, gathering information about treatment protocols offered in Boston, New York, Baltimore, Philadelphia. As the sun made its way across the country, I shifted my focus to facilities in the South, the Midwest and then Texas. By the time 9 a.m. rolled around, when they started answering phones at offices in L.A. and San Francisco, Palo Alto and Seattle, I had already filled pages in my legal pads.
I’d been a journalist in my younger years, but nothing in my life — or anyone’s who isn’t a medical professional — prepares a person to make the life decisions we faced then, with the knowledge that you get only one shot at this. Choose a poor option, and the person you love will die. Choose a better option, and more than likely that’s still the story. But I never allowed myself to see that. A lifelong optimist (whereas Jim, an attorney, had trained himself to anticipate worst-case scenarios), I was the voice of hope, and maybe because Jim had so much love and respect for my opinions on things, he adopted my belief that this cancer was survivable, and that he would survive it.
‘Pay me what you think this visit was worth,’ he said. Though money was tight, I wrote a check for $1,000. That’s how hard I wanted to believe.
I became an unrecognizable person. Or maybe just the same person in unrecognizable circumstances, which sometimes gave me the appearance of a crazy person. I’d be partway into a conversation and suddenly realize I was talking at double speed. When it got too late to make any more phone calls, I stayed hunched over my laptop planning the next day’s assault on the tumor. Even with the lights out, lying in bed — my right hand on Jim’s belly, in the place where the tumor was situated, sending out vibrations to Go Away — I couldn’t stop thinking about it.
Living in the Bay Area, we have two world-class medical facilities close by, but I was fixated on scouring the globe for a place to go that might save Jim. I know now what propelled me on my quest. It was a kind of magical thinking, that if we worked harder than everyone else — traveled farther, upended our lives more drastically, subjected ourselves to more hardship, even — we might tip the odds in Jim’s favor.
Early on in our battle, we made a pilgrimage to Los Angeles — a seven-hour drive, Jim on heavy painkillers — to consult an oncologist known for his highly unconventional use of an off-label form of chemotherapy: $6,000 per infusion, not covered by insurance, the use of which, he claimed, offered greater chances for shrinking a tumor in the pancreas. When our visit was over, and we took out our checkbook, I asked what we owed him for our consultation.
“Pay me what you think this visit was worth,” he said. Though money was tight, I wrote a check for $1,000. That’s how hard I wanted to believe.
In the end, we settled on a medical team in Boston, 3,000 miles away from home, to oversee Jim’s treatment. This included chemotherapy infusions locally and monthly checkups on the other side of the continent — augmented by daily doses of reishi mushroom capsules, massive quantities of pomegranate seeds, twice-daily shakes with so many ingredients they took up our entire kitchen counter, and Touch for Health treatments that would have caused the old Jim (a total believer in pure science) to roll his eyes. I told him he should stop reading about the election (too stressful) and play more guitar. I didn’t really believe those things would cure the cancer, but I wanted my husband to have every single good thing going for him.
After eight months of treatment, we got the news: The tumor had shrunk by 50 percent. Our Boston surgeon was ready to operate.
The day before the surgery, we took in a game at Fenway Park. Jim was looking better than he had in months — no doubt thanks to a six-week break from chemotherapy and radiation. His hair was back; the neuropathy that had prevented him from playing his bass had disappeared; and his appetite was good enough — or maybe it was just his hunger for life — that we finished off a plate of two dozen oysters after the game, and when those were gone, ordered another dozen.
“It’s an odd thing,” Jim said on our way home from the ballpark. “Tomorrow I’m electing to have a surgery that will gut me like a fish. Right now all I want is to go off and live my life instead of checking into this hospital.
“But this is the last train out of the station,” he said. “I’m going to be on it.”
Through all of this, Jim continued to believe in the possibility of his survival, and looked to me as the source of that conviction.
That was Jim’s last day without pain. Our surgeon got the tumor out — a success, in his book — but Jim was hospitalized more than a dozen times over the following year with a long list of complications that included portal vein hypertension and two bouts of Clostridium difficile infection.
The latter were treated (outside our hospital’s protocol) with fecal transplant, the first of which (when we were told the next available appointment with a qualified gastroenterologist was weeks away) was administered at home by me, following the instructions of a YouTube video. Both times, the fecal transplants knocked out the C-diff within hours. But by the time the C-diff was effectively eradicated, Jim’s adjuvant chemotherapy had been interrupted for too long. No more chemotherapy, they told us. We knew enough by then to understand this was not good news.
Eight months after surgery — with Boston behind us now — Jim’s tumor markers began to rise. There was no point getting a scan to check for a recurrence, because then he got an infection in his liver, and for the next four months — months in which Jim spent more time in the hospital than out of it — the infection endured, and mutated. Ignorant as I was at the time, I actually said, early on during this period, “At least it’s just an infection, not a recurrence” — not recognizing that the one served as indication of the other.
Through all of this, Jim continued to believe in the possibility of his survival, and looked to me as the source of that conviction. Where once he had focused all efforts on qualifying for the Whipple, now his hopes lay in vanquishing the infection out of the hope (to this it had come) that he might receive more chemotherapy.
On a visit during this period, Jim’s oncologist asked him the routine question, “How are you feeling?”
“Really great,” he told her.
I studied my husband’s ravaged face. Jim had always been an unswervingly honest man, an Eagle Scout, both figuratively and literally, and he wasn’t feeling remotely great or even OK. But I knew what he was doing, and didn’t challenge him. He just wanted, so badly, for our doctor to sign off on another round of chemo.
She didn’t. Chemo now would kill him, she said. Not that the cancer wasn’t doing that already.
In the car on the way home, I tried to ease the blow of our oncologist’s decision. “Maybe it’s better this way,” I said to Jim — the words among the hardest I ever spoke. “We know chemotherapy can’t cure Stage 4….”
My husband looked at me with baffled amazement. Way back when we’d started all this, we’d read the same articles, knew the same medical facts. Now (under the influence of morphine, and the cumulative effects of Folfirinox) he’d forgotten, and it fell to me to remind him that his doctors had nothing left for him.

My husband died a year and a week after undergoing the long-sought-after Whipple procedure. He was at home, in our bed. I was beside him.
Questions and an answer
I have spent the year since Jim’s death trying to make sense of the choices Jim and I made (though increasingly, they fell to me, alone) concerning his treatment. It is a terrible responsibility for any human being, but particularly one with no medical background, to make the kinds of choices I did for my husband. The fact that we had known each other only three years when he was diagnosed did not alter my love or commitment, but it did contribute to an uncharacteristic level of self-doubt.
Since Jim died, I have gone back over everything we did, asking myself what I might have done differently. The fact that he almost certainly would have died, regardless, does not mitigate the question of whether I might have made it possible for him to have known a less brutally painful final year.
Here is one thing I know, though it is a lesson acquired only through suffering and loss. If, tomorrow, or next week, or anytime in the next 30 years, I receive a diagnosis of pancreatic cancer, with the option existing for surgery, I would never elect to undergo the Whipple procedure. Whatever slim prospect of survival it might offer does not offset, for me, the countless complications, indignities and virtually nonstop pain I witnessed in my husband.
Of all the brutal experiences Jim endured over the 19 months of his cancer battle, none was harder for him than arriving at the place where hope no longer existed.
But there is a profound question underlying a decision like this one, and each individual might answer it differently. Does a patient like Jim do better to surrender to the virtual inevitability of his own death or — as my husband chose — go down fighting, almost to the end? I can guess that without that Whipple surgery, Jim might have gotten another good six months, maybe nine — months we might have spent riding those bicycles of ours and eating good meals, sitting in our garden together, taking walks, with surprisingly little pain. Except the ever-present grief of knowing what lay ahead.
Instead, we spent Jim’s last year engaged in constant, often excruciating struggle. We traveled some, and we still danced in our kitchen almost to the end, but it would not be much of an exaggeration to say that the fight to stay alive was killing us.
For a brief time, we made an hour-long drive each way, three times a week so Jim — who struggled with claustrophobia — might lie for 90 minutes in a hyperbaric chamber ($450 per visit) in the hope that doing so would diminish the infection overtaking his liver. The idea was that by accomplishing this, he might qualify for chemotherapy that would no longer offer any prospect of saving his life. Only extending it. Perhaps.
I was the one, in the end, who suggested that we stop this. Jim might have continued, though he was down to 90 pounds, and had already survived a nearly fatal septic episode that had me driving over the Bay Bridge to the hospital at midnight with my delirious husband.
I have asked myself, was I crazy?
Nobody was making me do this, or trying to make a buck off of Jim’s condition (though, of course, many people did make a buck off our increasingly desperate and wild pursuits). I made the choices I did out of the belief that for this particular man, in his particular situation, great pain, or dislocation, or even agony remained more endurable than the evaporation of all hope.
This belief was confirmed for me when we finally gave up all our efforts and — once again at my suggestion — went on hospice. Of all the brutal experiences Jim endured over the 19 months of his cancer battle, none was harder for him than arriving at the place where hope no longer existed.
For Jim, surrender was possible only when there was truly nothing else to be done. I do not consider him less spiritually evolved for his inability to view death as a valuable life experience. One could call him “in denial” about death. But I don’t think it was dying that he hated so much as it was leaving me.
From those first days after I met him, he was my guard dog, and the fight he undertook came out of his fierce commitment to remain at my side, no matter what. I see him now, in my mind’s eye, like one of those hero foot soldiers from long-ago wars, marching into battle to almost-certain death — the bullets whistling past his head, with one surely destined to fell him. He did not break his stride.
Best-selling author Joyce Maynard wrote this essay for Stanford Medicine about events in her memoir The Best of Us, to be published in September by Bloomsbury USA. Contact her at joycemaynard.com.
In this 1:2:1 podcast, best-selling author Joyce Maynard talks about helping her husband battle cancer, their love, and how his final months changed her.