Desegregating hospitals
How Medicare’s architect forced hospitals to admit Black people
The landmark Civil Rights Act of 1964 outlawed segregation and discrimination on the basis of race, religion, gender or national origin. Another milestone of the civil rights movement came the following year: the establishment of Medicare — and the end to hospitals nationwide turning away patients because of the color of their skin.
Related story
“Righting decades of wrong” describes projects in which Stanford Medicine researchers and physicians are involved to help counter the impact of racism on health.
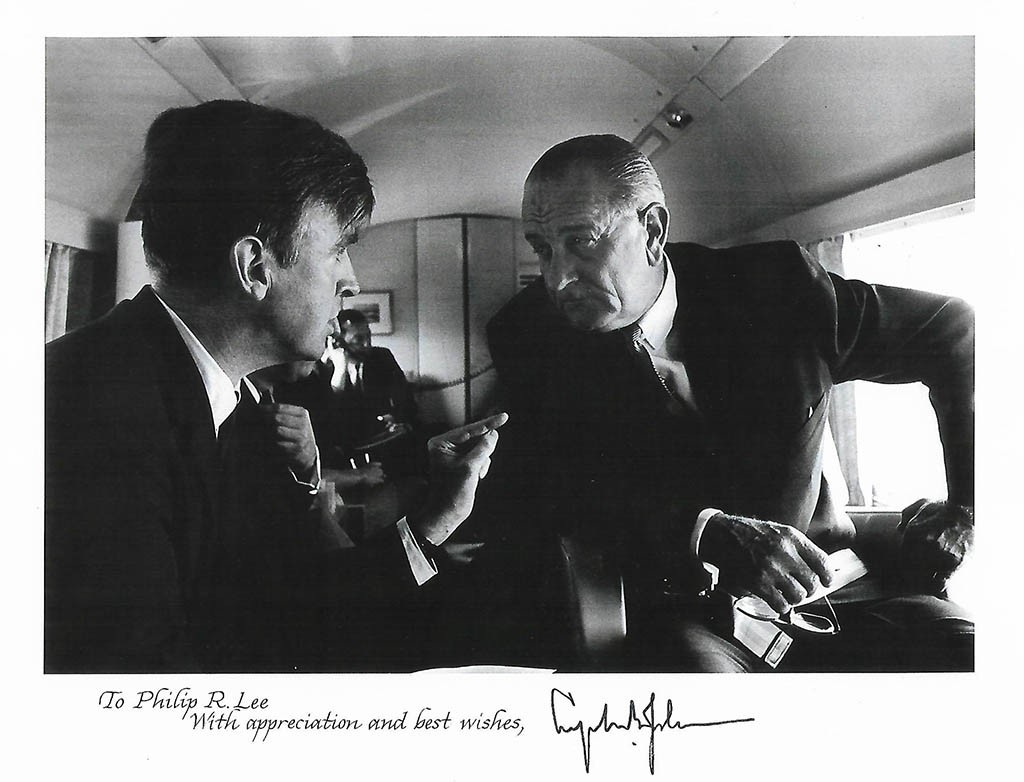
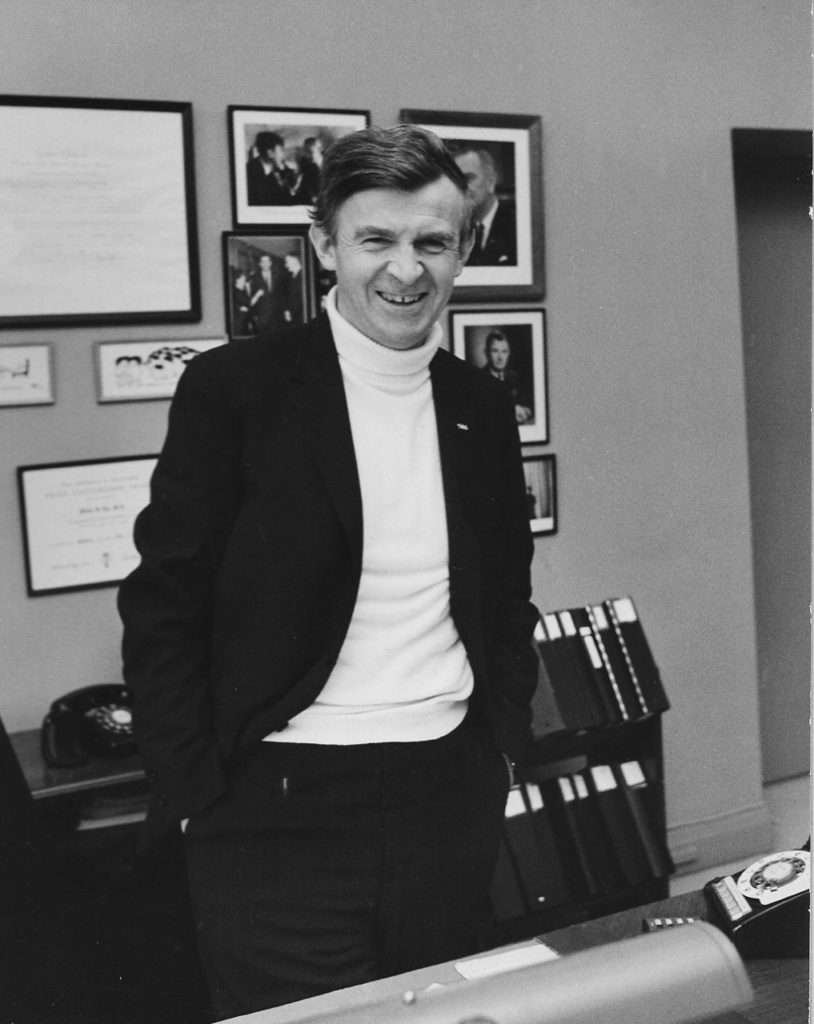
Medicare was the crown jewel of President Lyndon B. Johnson’s Great Society, a set of programs aimed at ending poverty and racial injustice. Johnson’s assistant secretary of health, Philip Lee, MD, championed the cause by insisting that hospitals receiving the new Medicare funding for their elderly patients follow the Civil Rights Act by ending discrimination against their patients on the basis of race.
His role as the architect of Medicare — and in telling some 7,000 hospitals, “No Black patients, no Medicare funding” — would become his greatest legacy. Lee, a graduate of the Stanford University School of Medicine, died in October at the age of 96.
In a 2015 article in the Journal of the American Society on Aging, Lee wrote that in 1965 a cardiologist at Georgia Baptist Hospital told him that if he put a Black patient in with a white one, his white patient “would die of a heart attack.”
Lee responded to him and other hospital administrators who balked at admitting Black patients: “Well, it’s the law; there’s going to be no Medicare money if the hospital doesn’t desegregate.” By February of 1967, Lee wrote, 95% of hospitals were receiving Black patients.
“For Phil, it was a powerful tool to address the racial and economic injustices that plagued America at the time,” said his nephew, Peter Lee, executive director of Covered California, the state’s health-care marketplace under the Affordable Care Act.
In the early 1960s, Philip Lee had lobbied in support of a precursor to Medicare — in opposition to the American Medical Association. He and LBJ took the political high road in making Medicare and Medicaid funding contingent on desegregation, said Peter Lee. “Money talked — and most hospitals changed their policies almost overnight.”
After several senior government roles, Philip Lee returned to California as director of UC San Francisco’s Institute for Health Policy Studies and later served as UCSF chancellor. He also taught graduate seminars in health policy at Stanford.
“Dr. Lee was one of the great leaders in American health policy,” said Stanford School of Medicine professor Laurence Baker, PhD. “The Medicare program, which he played an instrumental role in implementing, went on to transform access to health care for elderly and disabled Americans, and he had a hand in shaping every piece of our health care delivery system.”

