Beyond climate dread
Striving to improve health during the environmental meltdown

When you think of the climate crisis and the major impact it will have upon all corners of the world, one nation stands out as the epicenter of the unfolding cataclysmic changes: Bangladesh.
When Stephen Luby, MD, began working there two decades ago, the South Asian country was facing tremendous climate stress brought on by intermittent floods, extreme heat, cyclones and drought that threatened human life.
But as bad as it was then, the impact of climate on people’s health there has become progressively worse, said Luby, an epidemiologist who worked for the U.S. Centers for Disease Control and Prevention in Bangladesh before joining the Stanford School of Medicine’s faculty.
With shrinking land caused by the rising sea levels and changes in river flows that are reducing fresh water supplies, the low-lying nation is reaching a point where it will no longer be able to produce enough food for its people, he said.
At the same time, the weather has become erratic. As one of the world’s most densely populated countries with large portions near sea level and thus prone to flooding, Bangladesh is considered a canary in a coal mine for the climate crisis.
“For centuries we had dry years and wet years, but it was a stable system. More recently, though, greenhouse gas emissions, destructive land use and damaging fertilizers have pushed the country outside the area where it can come back into balance,” he said. “We are biological creatures, and we have not tended to our life-support system — the health of the planet — in ways we need to.”
Luby is among a growing number of Stanford Medicine community members dedicated to finding solutions to these urgent problems of planetary and human health.
“I do think we have an obligation because we are one of the world’s leading universities and this is the great crisis of our time,” said Luby, who’s also a senior fellow at the Stanford Woods Institute for the Environment.
“We are biological creatures, and we have not tended to our life-support system — the health of the planet — in ways we need to.”
Stephen Luby, MD, a senior fellow at the Stanford Woods Institute for the Environment
As signatories to the Biden administration’s new climate pledge to cut greenhouse gas emissions by 50% by 2030 and eliminate them altogether by 2050, Stanford Medicine leaders are working toward greater planetary health and health care sustainability.
Though Stanford Hospital and Lucile Packard Children’s Hospital Stanford have been certified as among the country’s most sustainably constructed hospitals, the institutions leaders continue to scrutinize every aspect of operations — from heating and cooling, to supply chain management and even food services — to limit their carbon footprint.
“One of the primary reasons for Stanford Medicine to move very assertively into sustainability is that we can be a role model,” said Helen Wilmot, chief facilities and sustainability officer at Stanford Health Care. “Not only do we have the resources, but we also have the intellectual energy — people who want to make a difference on this issue.”
Christy Foster, the director of sustainability at Stanford Medicine Children’s Health, said the need for action became starkly apparent after she and her colleagues took part in the first annual Global Climate Action Summit at Stanford in 2020.
“It was this ‘aha’ moment,” Foster said. “We all had evidence that the climate crisis was a problem, but it was also having an impact on the very patients we were trying to heal.”
She said climate change was no longer an abstract concept, as California was facing multiple weather emergencies — extreme summer heat and some of the worst wildfires in decades caused by intensifying drought — that led to an influx to Northern California hospitals of children with severe respiratory problems and pregnant women suffering heatstroke, high blood pressure and other problems.
“I feel we have a responsibility to deliver the same quality of medicine that we have for years, but we have to do it in a way that minimizes our impact, both locally and globally,” she said.
Index of topics in this article:
- DANGEROUS DUST: Dirty air is a major threat to children’s health in sub-Saharan Africa
- CONSERVING WATER: Quantifying, modeling and optimizing water use for hospitals
- A MOSQUITO’S DREAM: Cleaning up plastic trash in Kenya to eliminate mosquito-borne illness
- CLIMATE ANXIETY: Overcoming the next generation’s climate dread
- GREEN CEMENT: Replacing dirt floors with concrete in Bangladeshi homes — sustainably
- OCEAN-FRIENDLY SUNSCREEN: Formulating ocean-friendly sunscreen
- MAKING WASTEWATER DRINKABLE: Engineering a way to turn wastewater into purified drinking water, ammonia and other useful materials
Consequences for human health
Michele Barry, MD, director of the Stanford Center for Innovation in Global Health, has seen firsthand how changes in the environment have affected people’s health, particularly in low-income countries. For instance, outbreaks of many of the hemorrhagic viruses — such as Ebola, which she has studied — are a result of land clearing for crops and domestic use that put humans in close contact with animals carrying deadly viruses.
“We have definitely seen spillover incidents such as the Ebola epidemic happen as our land use changes and we encroach on animal habitats,” said Barry, a tropical disease doctor.
Additionally, climate change is leading to new patterns of disease and placing at risk global food supplies, water, personal safety and mental health, she said.
“I think we are on red alert. It should be all hands on deck with what is happening in our climate,” she said. “When the new normal in California is atmospheric rivers and excessive wildfires, that should be a wake-up call domestically. Globally we’re seeing huge shifts of disease due to climate and distribution of vectors like mosquitoes and ticks.”
Her center identified it as a top priority in 2017 and funds dozens of initiatives to address the problem — from projects in South Asia to reduce coal consumption to studies of how dams and other agricultural systems are causing a rise in parasitic diseases.
Projects and programs aimed at solutions
Stanford Health Care supports research projects that address the problem locally. Nine faculty and staff have received funding under the health system’s Seed Grant Program for Sustainability to find ways to reduce the carbon footprint of Stanford Hospital operating rooms, minimize waste in the emergency department and reduce hospitalwide water consumption.
In addition, five nurses are using funds from the Stanford Health Care Sustainability in Nursing Fellowship to examine various methods to minimize waste, reuse products where possible and reduce employee commutes, among other projects.
The Stanford School of Medicine is co-sponsoring a program for redesigning living systems to tackle sustainability challenges. Seed grants for Synthetic Biology for Sustainability support multidisciplinary groups of researchers who can build or modify cells, molecules, organisms or other biological systems with the aim of solving environmental problems. The program is a joint effort with the School of Engineering and the Doerr School of Sustainability.
Luby is spearheading the creation of a Center for Human and Planetary Health within the Doerr School in a collaboration between the Woods Institute and the Center for Innovation in Global Health. He envisions it as an opportunity for environmentalists and physicians to collaborate on improving the health of humans and the Earth.
He is continually motivated by students who are profoundly concerned about the planet’s future, he said.
“We have to think beyond climate dread. People are feeling disempowered and frustrated, and they turn to us and say, ‘Where do we go? What do we do?’” he said. “We have a responsibility to give them a toolkit so they can advance solutions. We can train the workforce and motivate people so that we are all solution oriented.”
The following examples illustrate how members of the Stanford Medicine community are striving for solutions.
DANGEROUS
DUST
Desert dust: a major threat to children’s
health in sub-Saharan Africa
Eran Bendavid, MD, was studying the effects of global warming on child health when he realized there was a far bigger environmental threat to kids: dirty air.
While poring over health data on a million children in sub-Saharan Africa, Bendavid and his colleagues discovered that poor air quality is as great a risk to the region’s children as major killers like malaria or the flu, he said.

“We found that 15-20% of infant deaths were linked to poor air quality,” said Bendavid, an associate professor of medicine and a senior fellow at the Woods Institute for the Environment. “We start seeing adverse effects as soon as air quality starts deteriorating. It raises the risk of pneumonias, stunted growth and other factors that increase a child’s risk of death.”
While air pollution in sub-Saharan African countries includes obvious sources like burning trash, indoor cooking and brush fires, one major source is underappreciated: dust that drifts from the Sahara Desert.
“Parts of the Sahara raise some of the world’s biggest dust storms. They are so large that they cross the Atlantic Ocean and can be measured in the Amazon,” he said. “When those dust storms pick up, it makes a big difference for air quality in most of Central and Western Africa, and it impacts these very young children who are especially vulnerable in the first year of life.”
Experts predict that these storms will become more frequent and severe because of drought conditions brought on by climate change. The particulate matter from Saharan dust could account for as much as 24% of infant mortality, Bendavid and collaborators, including Stanford University environmental scientists Sam Heft-Neal, PhD, and Marshall Burke, PhD, reported in a 2020 study in Nature Sustainability.
The scientists suggested using underground water sources to dampen the surface of the desert, a technique found to be effective on a small scale in California, Bendavid said.
“We propose to pump a little bit of water from groundwater wells to improve the dust conditions in those areas,” a low-cost solution, he said.
EVENT: The Stanford Medicine Center for Excellence in Pulmonary Biology and Stanford Children’s Hospital are holding a symposium — When Helping Kids Means Healing the Planet: Climate Change and Childhood Lung Health — on June 19, 2023. Click here to find out more and register.
CONSERVING WATER IN HOSPITALS
Quantifying, modeling and optimizing
water use for hospitals and patients
with cancer
A Native Hawaiian, Kekoa Taparra, MD, PhD, grew up surrounded by water and appreciating the value of this precious resource. Now, he’s researching ways to conserve it in one of the nation’s top water-consuming industries: hospitals.
Among commercial buildings, hospitals are the country’s leading users of water, with a 2017 U.S. Energy Information Administration study finding that they use more than double that of all large buildings in the country, Taparra said. Hospitals require water for cooling and heating, plumbing, cleaning and maintaining equipment, among other activities.
“We really have to be intentional about the water used throughout the hospital and per patient,” said Taparra, a third-year radiation oncology resident, noting that water is becoming an increasingly scarce global commodity.
Unlike electricity, there is no metric or “gold standard” on acceptable levels of water consumption in hospitals, and there is little understanding of how much water is used or wasted in the medical care system. He hopes to help fill the gap through a new project at Stanford Health Care to quantify water use and see how that compares with other non-hospital facilities.
Supported by a 2022-2023 Stanford Health Care Sustainability seed grant, Taparra has developed a three-part approach to evaluating water use in hospitals. First, he has gathered data from 2018 to 2022 for seven hospital and clinic facilities and plans to contrast that with water usage in non-hospital buildings on campus and across the country.
He’s also developing a model of how seasonal variations in temperature and hotter weather have affected hospital water usage: “With average temperatures rising and the occurrence of increased instances of heat waves, are we using more water in our hospitals?”
Finally, he plans to measure water usage in the Department of Radiation Oncology, where clinicians use technologies that deliver energy to target and kill cancers, producing heat as a byproduct. These machines must be constantly cooled with chilled water, so Taparra plans to install a meter to gauge the flow to compare water use between different radiation therapy machines.
A leader in the field of radiation oncology, Stanford Medicine recently installed some next-generation machines for advanced cancer treatment, he said. “Stanford is known for these unique technologies, but we must ask, are they sustainable?” Taparra hopes to have some answers by early 2024.
PLASTIC: A
MOSQUITO’S DREAM
Cleaning up plastic trash in Kenya
to eliminate mosquito-borne illness
Desiree LaBeaud, MD, who has conducted epidemiology research in Kenya for two decades, was speaking to a group of Kenyan school children several years ago, when a previously unrecognized source of disease suddenly came into focus.
“I asked the students, ‘Where do you see the mosquito vectors?” which are major breeders of many important infectious diseases. “They said, ‘In the piles of trash behind our homes and schools.’”
Man-made containers like plastic bottles are a primary source of disease-carrying vectors in many low-income countries like Kenya, as they provide the ideal habitat for the Aedes aegypti mosquito, which spreads dengue, chikungunya, Zika and yellow fever viruses.

In early 2021 in south coastal Kenya, LaBeaud, a pediatric infectious disease specialist, developed a community nonprofit, the Health and Environmental Research Institute-Kenya, to educate people in the community about the environmental and health hazards of leaving plastic lying around and mobilize them to recycle, reuse or remove it. HERI-Kenya is supporting the creation of circular economies of waste to find solutions to the ongoing pollution crisis and create local economic opportunities and jobs from this unlikely resource.
“There is no formal recycling here, only an informal recycling trade, so plastic has little value on the market,” said LaBeaud, a professor of pediatrics, a senior fellow at the Woods Institute for the Environment and an adviser at the Center for Innovation in Global Health. “About 75% of it is burned, creating toxic pollutants, or finds its way into oceans, choking marine life, or on land where it breeds mosquitoes. This is a problem not just in Kenya but in most of the world.”
The nonprofit aims to empower community members, scientists and policymakers to create a culture of sustainability while building expertise in environmental health research with the ultimate goal of improving community health, said LaBeaud, who is on sabbatical in Kenya to focus on the organization. In April, the group opened an environmental learning resource center to train people in waste management, circular economies and eco-friendly practices.
And it is organizing regional community groups composed of varied stakeholders — from local business and government to nonprofits and recyclers — to implement new community-based initiatives and find local solutions.
Through the organization, whose acronym HERI means blessed or happy in Swahili, community members conduct beach and urban cleanups and plant trees. They also plan to work with recyclers to turn durable plastics into building products like pavers, roofing tiles and bricks, she said.
With a grant from the Stanford Visiting Artist Fund in Honor of Roberta Bowman Denning, the nonprofit commissioned artist Jean Shin to create two sculptures out of plastic waste to highlight the plastic pollution crisis. In Kenya, the organization hired more than 50 residents to transform more than 7,000 single-use plastic water bottles into a massive wave.
The sculpture was unveiled in the center of the Diani/Ukunda urban area on Earth Day 2023. The second sculpture will sit in the Biomedical Innovations Building on the Stanford Medicine campus.
THE GREENING
OF CEMENT
A sustainable approach to replacing
dirt floors with concrete in Bangladesh
Millions of the world’s children grow up crawling around and playing on dirt floors, which can hide disease-causing bacteria and parasites, including soil-transmitted helminths. These worms lodge in the intestine and can cause persistent diarrhea, pain and malnutrition and can slow physical and cognitive growth.
Jade Benjamin-Chung, PhD, an assistant professor of epidemiology and population health, is experimenting with a sustainable approach to eliminating this risk and improving the long-term health of children and their mothers.
Before coming to Stanford Medicine, Benjamin-Chung worked with Luby as an epidemiologist in Bangladesh and saw the hardships of life in homes with dirt floors. Now she has a National Institutes of Health grant to replace dirt floors in some Bangladeshi homes with concrete, then measure the impact on the health of the children and their mothers. She said she believes the concrete floors could significantly lower infection rates.
But in planning the study, she decided to use a low-cost “green” form of cement — one of the key ingredients in concrete — in the interest of long-term sustainability. The production of such green cements emits less greenhouse gas than production of traditional cements.
The manufacturing of cement is one of the leading causes of greenhouse gas emissions and a major source of global pollution, she said. At least 8% of global carbon emissions caused by humans come from the cement industry, according to a 2021 article in the journal Joule by Imperial College London professor Paul Fennell and others.
“One of my engineering colleagues who is collaborating on this study encouraged me to look into these novel, green cements that could even be produced with existing materials,” Benjamin Chung said.
She obtained a Woods Institute for the Environment grant to experiment with different concrete ingredients, including fly ash, an often-discarded byproduct of coal processing.
The researchers are planning to enroll 800 households in rural Bangladesh in a study that will test the green floors against traditional concrete and dirt in a subsample. The participants will all be pregnant women whom researchers will follow for two years as they give birth to and raise their children.
They will test the children and the homes for parasitic worms and other infectious agents, while assessing the mothers for depression, stress and quality of life. Benjamin-Chung speculated that the mothers’ health will improve because they will find it easier to cook on and clean a concrete floor and will feel better generally about their home environment.
“The overarching question involves the health of the children and their mothers, but we are also taking planetary health into consideration from the very beginning,” she said. “I hope this will be a template for future studies that will encourage researchers to consider potential impacts of health interventions on the climate.”
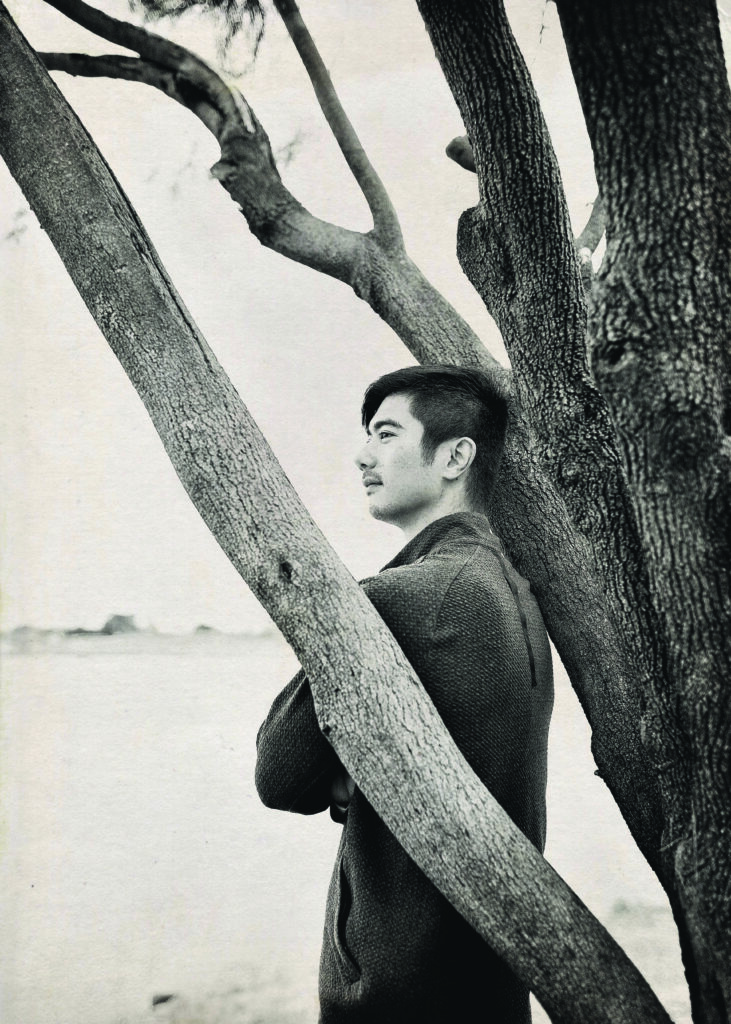
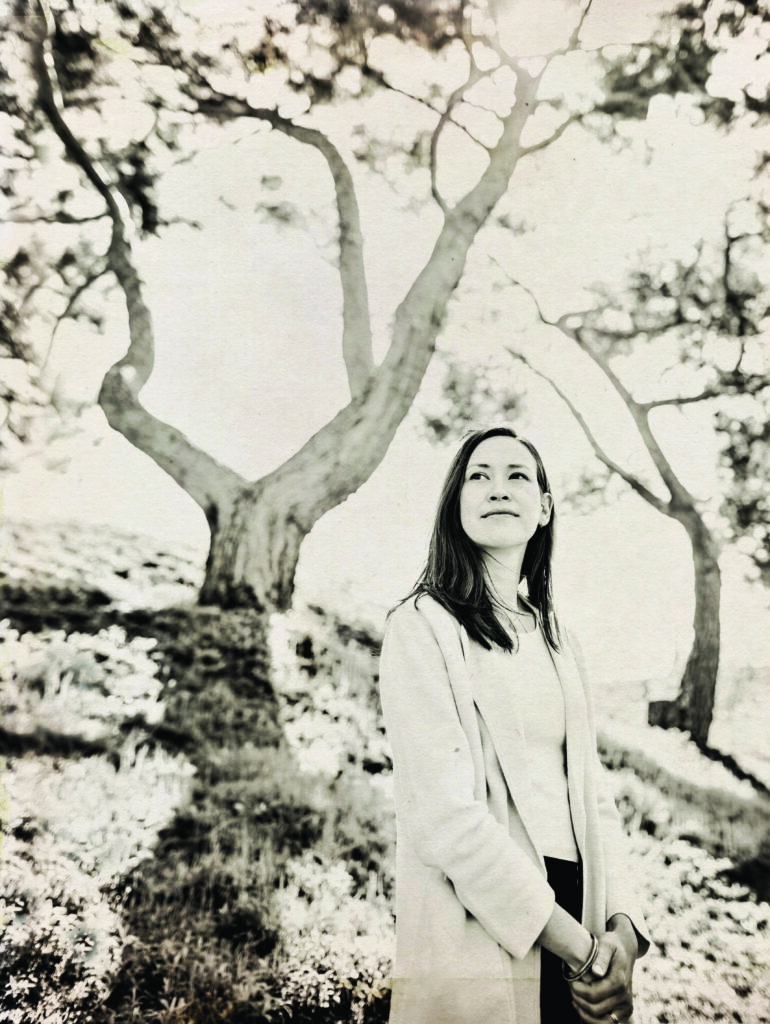
CLIMATE ANXIETY
Overcoming the next
generation’s climate dread
In 2021, Britt Wray, PhD, co-authored a study of more than 10,000 young people in 10 countries who said they were profoundly anxious about climate change. About three-quarters said the “future is frightening,” and half experienced climate dread to a degree that affected their daily lives, according to the study in Lancet Planetary Health.
At the same time, they said they felt betrayed by an older generation they perceive as not understanding their plight or combating the crisis.
Wray, an expert in science communication and the mental health impacts of climate change, is trying to bridge that divide in a project that brings together people of different generations to share concerns and experiences and chart a path for change.
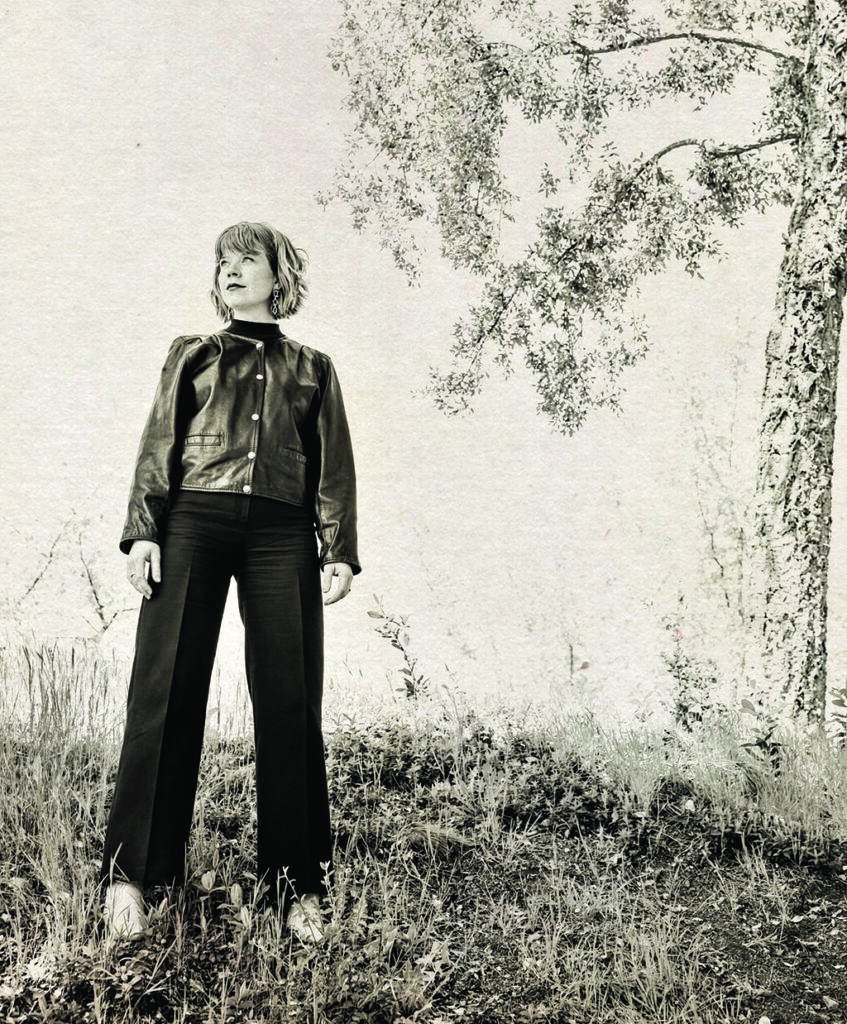
“We thought if we could bring young people into a meaningful relationship with elders who do care and are hungry for action, that could potentially be therapeutic and useful in a number of ways,” said Wray, an instructor in the Department of Psychiatry and Behavioral Sciences, who is leading the Special Initiative of the Chair on Climate Change and Mental Health.
From November 2022 through February 2023, small multigenerational groups in three countries — Nigeria, England and the United States — met once a month over Zoom to express how the crisis is affecting their psychological well-being. A community facilitator guided the conversations to create a supportive environment where people could talk openly.
Wray sat in on all the conversations in New Orleans with people who are still grappling with psychological trauma from Hurricane Katrina, the 2005 storm that devastated the city, she said.
“People don’t even have the vocabulary to recognize the emotional impact — the degrading sense of security — that the climate crisis has created,” Wray said.
In Nigeria, she observed a strong sense of coming together over the crisis, while in London, there was friction among the participants, with some older people saying they believed global climate change was “not that big of a deal,” she said.
The recorded conversations are now being analyzed by Wray’s team using the Local Voices Network technology platform, created by the MIT Media Lab, that uses machine learning to identify key, meaningful themes.
Wray believes these kinds of small group conversations, replicated in hundreds of locations around the globe, can empower communities as they cope with the psychological impact of the crisis and forge connections to take action.
OCEAN-FRIENDLY
SUNSCREEN
Formulating a sunscreen alternative
that won’t harm ocean life
More people are using sunscreen to protect their skin, with the U.S. sunscreen market projected to grow from $1.8 billion in 2014 to $2.4 billion by 2025, market studies show. But these sunscreen users may be unwittingly putting ocean life at risk.
The active ingredients in most approved products, such as zinc and oxybenzone, are toxic to marine life and are particularly damaging to coral reefs, said Paul Bollyky, MD, PhD, a Stanford Medicine immunologist and infectious disease specialist. (Despite its reef-friendly reputation, zinc oxide causes coral bleaching, which damages the algae on which the coral depend.)
Bollyky, an associate professor of medicine, and his collaborator Giulio De Leo, PhD, a Stanford Doerr School of Sustainability professor of oceans and of Earth system science, are investigating a new ocean-safe alternative that is based on bacteriophages — viruses that can infect bacteria but not humans.
Bollyky is an expert on bacteriophages, the most abundant organisms on the planet. While studying how these organisms interact with light, he and his colleagues found that some are very good at absorbing ultraviolet light, which is also what sunscreens do to protect human skin from these harmful rays. Bollyky speculates that these bacteriophages evolved to absorb or reflect UV light as a way to shield their own DNA.
The researchers engineered versions of these bacteriophages so they would not infect bacteria, then incorporated these UV-protective organisms into sunscreens, which mostly contain moisturizers and other agents to help them adhere to the skin.
“Our idea is to swap out the active ingredients in sunscreens that are toxic to ocean life and instead use bacteriophage particles,” said Bollyky. “Because they are organic, they will decay.”
The research team has measured these bacteriophage sunscreens for their ability to absorb UV light and has begun experimenting with them on human skin tissues. Next, they plan to test the protective effects of these new sunscreens in animal models, he said. If that proves encouraging, the scientists will collect safety and toxicity data as a prelude to a clinical trial.
The project is funded by a two-year grant from the Realizing Environmental Innovation Program at the Woods Institute for the Environment. His co-investigators are bacteriophage biologist and graduate student Julie Pourtois and materials scientist and postdoctoral fellow Maryam Hajfathalian, PhD — two team members with intersecting passions, Bollyky said.
MAKING WASTEWATER DRINKABLE
Engineering a way to turn wastewater
into purified drinking water, ammonia and
other useful materials
Polly Fordyce, PhD, is a geneticist whose lab has created a microchip able to analyze gene sequences at hyper-speed, shortening lab experiments by years. But in talking with colleagues across campus, she realized these tools could be applied to an entirely different problem: water purification.
Motivated by the increasing scarcity of clean water supplies, Fordyce and engineering experts Will Tarpeh, PhD, and Eric Appel, PhD, are collaborating on a new technology to reuse sewage. Based on current demand, the global need for drinking water will exceed supply by 40% by 2030, the researchers said.
“We’re asking, ‘How can you reuse water by getting rid of contaminants you don’t want while recovering materials that you could reuse?’” said Fordyce, an associate professor of genetics and bioengineering.
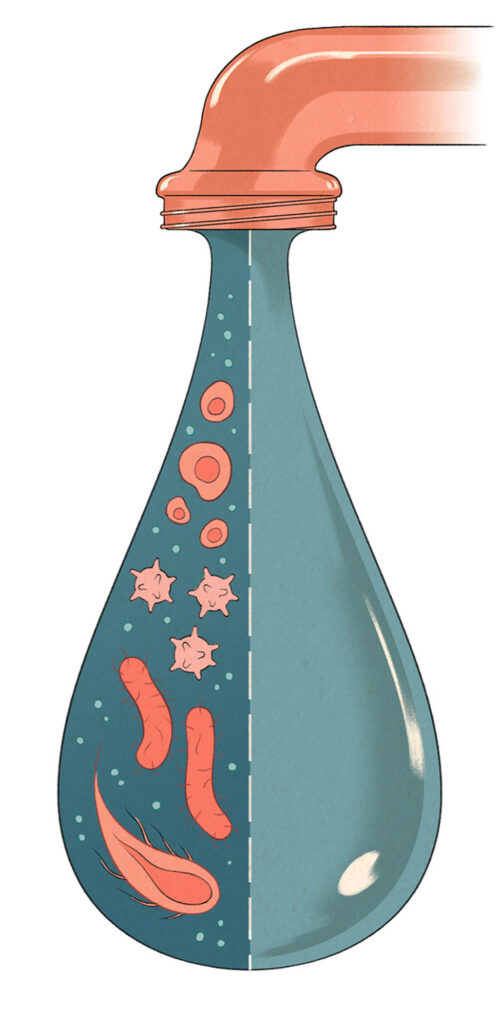
To do that, researchers are developing new resins — molecularly designed plastic beads — that will attach to specific contaminants in wastewater and act like a sieve to filter them out. Appel, assistant professor of materials science and engineering, plans to screen thousands of polymers — large molecules made of multiples of simpler chemical units — and combine them in different ways to create new resins.
Resin technology is well established in the wastewater treatment field, but it’s not selective for specific pollutants, said Tarpeh, an assistant professor of chemical engineering and a wastewater treatment expert.
“With the approach we are taking, you could make designer resins for any contaminant,” said Tarpeh, noting that these designer resins could also extract useful compounds, such as ammonia or phosphorous, which can be recycled and reused.
Fordyce’s role is to miniaturize the experiments, which will speed up testing. Instead of testing one resin at a time in large columns of fluid in the lab — the old method — her system enables the testing of multiple resins at once in more easily manageable micro droplets.
“That would help us find the right polymer more cheaply and faster,” Fordyce said.
The researchers’ goal is to produce resins that can be manufactured inexpensively in large quantities. They hope to attract industry partners and patent and commercialize these new technologies. The two-year project is funded by the Woods Institute for the Environment.

